Acute kidney injury
Overview
Acute kidney injury happens when the kidneys suddenly can't filter waste products from the blood. When the kidneys can't filter wastes, harmful levels of wastes may build up. The blood's chemical makeup may get out of balance.
Acute kidney injury used to be called acute kidney failure. Acute kidney injury is most common in people who are in the hospital, mostly in people who need intensive care.
Acute kidney injury ranges from mild to severe. If severe, ongoing and not treated, it can be fatal. But it also can be reversed. People in otherwise good health may get back typical or nearly typical use of their kidneys.
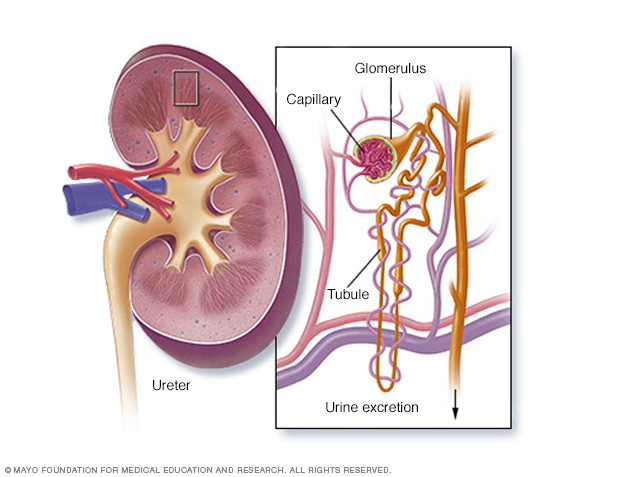
The kidneys remove waste and extra fluid from the blood through filtering units called nephrons. Each nephron contains a filter, called a glomerulus. Each filter has tiny blood vessels called capillaries. When blood flows into a glomerulus, tiny bits, called molecules, of water, minerals and nutrients, and wastes pass through the capillary walls. Large molecules, such as proteins and red blood cells, do not. The part that's filtered then passes into another part of the nephron called the tubule. The water, nutrients and minerals the body needs are sent back to the bloodstream. The extra water and waste become urine that flows to the bladder.
Symptoms
Symptoms of acute kidney injury may include:
- Less urine output.
- Fluid buildup, which can cause shortness of breath and swelling in the legs, ankles or feet.
- Tiredness.
- Confusion or fogginess.
- Nausea.
- Pain in the belly or in the side below the rib cage.
- Weakness.
- Irregular heartbeat.
- Itching.
- Loss of appetite.
- Chest pain or pressure.
- Seizures or coma in severe cases.
Sometimes acute kidney injury causes no symptoms. Then it may be found through lab tests done for something else.
When to see a doctor
See your healthcare professional right away or seek emergency care if you have symptoms of acute kidney injury.
Causes
Acute kidney injury can happen when:
- You have a condition that slows blood flow to your kidneys.
- You have damage to your kidneys.
- Your kidneys' urine drainage tubes, called ureters, get blocked.
Slowed blood flow to the kidneys
Conditions that may slow blood flow to the kidneys and lead to kidney injury include:
- Loss of too much body fluid, called dehydration.
- Infection with or without sepsis or septic shock.
- Medicines such as aspirin, ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve).
- Blood or fluid loss.
- Severe low blood pressure from blood pressure medicines.
- Heart attack.
- Heart failure or heart disease.
- Liver cirrhosis or failure.
- Bad allergic reaction, called anaphylaxis.
- Bad burns.
Damage to the kidneys
The following may damage the kidneys and lead to acute kidney injury:
- Swelling and irritation, called inflammation, of the tiny filters in the kidneys. This is called glomerulonephritis (gloe-mer-u-loe-nuh-FRY-tis).
- Medicines, such as certain chemotherapy drugs, antibiotics and dyes used during imaging tests.
- Infection, such as with the virus that causes coronavirus disease 2019 (COVID-19).
- Toxins, such as alcohol, heavy metals and cocaine.
- An immune system condition called lupus that causes glomerulonephritis.
- Blood clots in the veins and arteries in and around the kidneys.
- Cholesterol deposits that block blood flow in the kidneys.
- A condition that results from red blood cells being destroyed too early, called hemolytic uremic syndrome.
- A group of rare diseases affecting the skin and connective tissues called scleroderma.
- A rare blood disorder called thrombotic thrombocytopenic purpura.
- Muscle tissue breakdown, called rhabdomyolysis. The toxins from the muscle being destroyed leads to kidney damage.
- Breakdown of tumor cells called tumor lysis syndrome. This leads to the release of toxins that can injure the kidneys.
Urine blockage in the kidneys
Conditions that keep urine from leaving the body are called urinary obstruction. These can lead to acute kidney injury. They include:
- Kidney stones.
- Enlarged prostate.
- Blood clots in the urinary tract.
- Bladder cancer.
- Prostate cancer.
- Cervical cancer.
- Colon cancer.
- Growth pushing on the ureters.
- Nerve damage of the nerves that control the bladder.
Risk factors
Acute kidney injury almost always is linked to another medical condition or event. Conditions that can increase your risk of acute kidney injury include:
- Ongoing kidney disease, also called chronic kidney disease.
- Older age, but it does happen to children.
- Being in the hospital, most often for a serious condition that needs intensive care.
- Blockages in the blood vessels in your arms or legs, called peripheral artery disease.
- Diabetes, especially if it's not controlled.
- High blood pressure.
- Heart failure.
- Liver diseases.
- Certain cancers and their treatments.
Complications
Complications of acute kidney injury may include:
- Fluid buildup. A buildup of fluid in your lungs can cause shortness of breath.
- Chest pain. The lining that covers your heart, called the pericardium, can get inflamed. This can cause chest pain.
- Muscle weakness. This can result from the body's fluids and minerals in the blood called electrolytes being out of balance.
- Permanent kidney damage. Sometimes, acute kidney injury causes lifelong loss of the use of the kidneys, called end-stage renal disease. People with end-stage renal disease need either lifelong treatments to remove waste from the body, called dialysis, or a kidney transplant to survive.
- Death. Acute kidney injury can cause the kidneys to stop working.
Prevention
You might cut your risk of acute kidney injury by taking care of your kidneys. Try to:
- Get treated quickly for bad infections.
Work with your healthcare team to manage kidney and other ongoing conditions. Kidney disease, diabetes or high blood pressure increases your risk of acute kidney injury. If you have one of these, do what your healthcare team tells you to manage your condition.
If you have risk factors for kidney disease, check with your healthcare team to be sure that prescription medicines you take are safe for your kidneys.
- Read labels when taking pain medicines available without a prescription. Do what the label says when taking medicines such as aspirin, acetaminophen (Tylenol, others), ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve). Taking too much of these medicines may increase your risk of kidney injury. This is especially true if you already have kidney disease, diabetes or high blood pressure.
- Live a healthy lifestyle. Be active and eat a healthy, balanced diet. If you drink alcohol, drink only in moderation.
Diagnosis
You might have the following tests to diagnose acute kidney injury:
- Blood tests. A sample of your blood may show fast-rising levels of urea and creatinine. This helps show how your kidneys are working.
- Urine output measures. Measuring how much urine you pass in 24 hours may help find the cause of your kidney failure.
- Urine tests. A sample of your urine may show something that suggests a condition that might explain kidney failure. This is called urinalysis.
- Imaging tests. Imaging tests such as ultrasound and CT scans can show your kidneys.
- Removing a sample of kidney tissue for testing. Your healthcare professional may suggest removing a small sample of your kidney tissue for lab testing. This is called a biopsy. A needle put through your skin and into your kidney removes the sample.
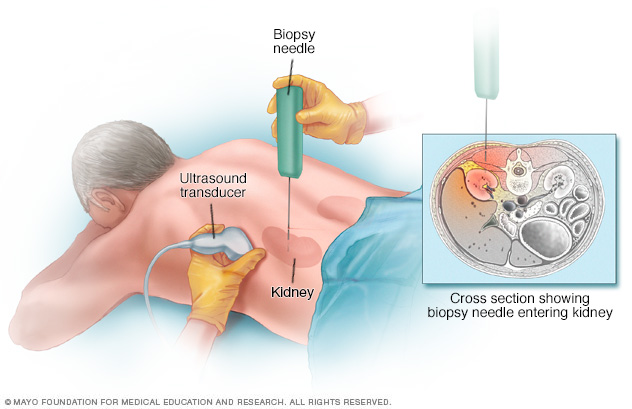
During a kidney biopsy, a healthcare professional uses a needle to remove a small sample of kidney tissue for lab testing. The biopsy needle is put through the skin to the kidney. The procedure often uses an imaging device, such as an ultrasound transducer, to guide the needle.
Treatment
Treatment for acute kidney injury most often means a hospital stay. Most people with acute kidney injury are already in the hospital. How long you'll stay in the hospital depends on the reason for your acute kidney injury and how quickly your kidneys recover.
Treating the cause of your kidney injury
Treatment for acute kidney injury involves finding the illness or injury that damaged your kidneys. Your treatment depends on the cause. It might involve stopping a medicine that's damaging your kidneys.
Treating complications until your kidneys recover
Your healthcare team also works to prevent complications and give your kidneys time to heal. Treatments that help prevent complications include:
Treatments to balance fluids in your blood. If a lack of fluids in your blood is the cause of your acute kidney injury, you may need fluids through a vein, called intravenous (IV) fluids.
If acute kidney injury causes you to have too much fluid, this may lead to swelling in your arms and legs. Then you may need medicines called diuretics, which cause your body to get rid of extra fluids.
Medicines to control blood potassium. Your kidneys might not filter potassium from your blood well enough. Potassium regulates blood pressure and other body functions.
You might need medicines called potassium binders to keep potassium from building up. These include sodium zirconium cyclosilicate (Lokelma) or patiromer (Veltassa). Too much potassium in the blood can cause irregular heartbeats, called arrhythmias, and muscle weakness.
- Medicines to restore blood calcium levels. If the levels of calcium in your blood drop too low, you might need to get calcium through a vein, called an infusion.
Treatment to remove poisons from your blood. If wastes build up in your blood, you may need hemodialysis for a time. Also called dialysis, it helps remove poisons and excess fluids from your body while your kidneys heal.
Dialysis also may help remove excess potassium from your body. During dialysis, a machine pumps blood out of your body through an artificial kidney, called a dialyzer, that filters out waste. The blood is then returned to your body.
Lifestyle and home remedies
During your recovery from acute kidney injury, a special diet can help support your kidneys and limit the work they must do. Your healthcare team may send you to a dietitian. A dietitian can look at what you eat and suggest ways to make your diet easier on your kidneys.
Your dietitian may suggest that you:
- Choose foods lower in potassium. These include apples, peaches, carrots, green beans and white bread and white rice. Eat them instead of foods higher in potassium. These include potatoes, bananas, tomatoes, oranges, beans and nuts.
- Don't eat foods with added salt. This includes many packaged foods, such as frozen dinners, canned soups and fast foods. Other foods with added salt include salty snack foods, canned vegetables, and processed meats and cheeses.
- Limit phosphorus. Phosphorus is a mineral found in foods, such as dark-colored sodas, milk, oatmeal and bran cereals. Too much phosphorus in your blood can weaken your bones and cause your skin to itch.
As your kidneys get better, you may no longer need a special diet. But healthy eating still is important.
Preparing for an appointment
Most people are in a hospital when they get acute kidney injury. If you aren't in the hospital and have symptoms of kidney failure, make an appointment with your family healthcare professional right away. You may be referred to a specialist in kidney disease, called a nephrologist.
Before your appointment, write down questions. Consider asking:
- What's the most likely cause of my symptoms?
- Have my kidneys stopped working? What could have caused my kidney failure?
- What tests do I need?
- What are my treatment choices, and what are the risks?
- Do I need to go to the hospital?
- Will my kidneys recover or will I need dialysis?
- I have other health conditions. How can I best manage these conditions together?
- Do I need to eat a special diet? If so, can you refer me to a dietitian to help me plan what to eat?
- Do you have printed materials about acute kidney injury that I can have? What websites do you suggest?
Last Updated Jul 10, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use




