Arteriovenous fistula
Overview
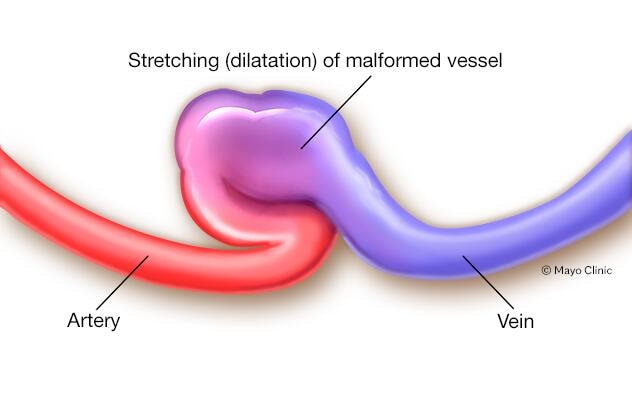
An arteriovenous (AV) fistula is an irregular connection between an artery and a vein. Usually, blood flows from the arteries to tiny blood vessels (capillaries), and then on to the veins. Nutrients and oxygen in the blood travel from the capillaries to tissues in the body.
With an arteriovenous fistula, blood flows directly from an artery into a vein, avoiding some capillaries. When this happens, tissues below the avoided capillaries receive less blood.
Arteriovenous fistulas usually occur in the legs but can develop anywhere in the body. An arteriovenous fistula may be surgically created for use in dialysis in people with severe kidney disease.
Symptoms of arteriovenous fistulas depend on where they form in the body. A large untreated arteriovenous fistula can lead to serious complications. Treatment for arteriovenous fistulas includes monitoring, compression, catheter-based procedures and, sometimes, surgery.
Symptoms
Small arteriovenous fistulas in the legs, arms, lungs, kidneys or brain often won't have any signs or symptoms. Small arteriovenous fistulas usually don't need treatment other than monitoring by a health care provider. Large arteriovenous fistulas may cause signs and symptoms.
Arteriovenous fistula signs and symptoms may include:
- Purplish, bulging veins seen through the skin, similar to varicose veins
- Swelling in the arms or legs
- Decreased blood pressure
- Fatigue
- Heart failure
A significant arteriovenous fistula in the lungs (pulmonary arteriovenous fistula) is a serious condition and can cause:
- Pale gray or blue lips or fingernails due to lack of blood flow (cyanosis)
- Fingertips to spread out and become rounder than normal (clubbing)
- Coughing up blood
An arteriovenous fistula in the digestive tract can cause gastrointestinal (GI) bleeding.
When to see a doctor
If you have signs and symptoms of an arteriovenous fistula, make an appointment to see your health care provider. Early detection of an arteriovenous fistula may make the condition easier to treat. It may also reduce the risk of developing complications, including blood clots or heart failure.
Causes
Arteriovenous fistulas may be present at birth (congenital) or they may occur later in life (acquired). Causes of arteriovenous fistulas include:
- Injuries that pierce the skin. An arteriovenous fistula may result from a gunshot or stab wound that occurs on a part of the body where a vein and artery are side by side.
- Congenital arteriovenous fistulas. In some babies, the arteries and veins don't develop properly in the womb. It's unclear exactly why this happens.
- Genetic conditions. Arteriovenous fistulas in the lungs (pulmonary arteriovenous fistulas) can be caused by a genetic disease that causes irregular blood vessels throughout the body, but especially in the lungs. One such disease is Osler-Weber-Rendu disease, also known as hereditary hemorrhagic telangiectasia.
- Dialysis-related surgery. People who have late-stage kidney failure may have a surgery to create an arteriovenous fistula in the forearm to make it easier to perform dialysis.
Risk factors
Certain genetic or congenital conditions increase the risk of arteriovenous fistulas. Other potential risk factors for arteriovenous fistulas include:
- Older age
- Female sex
- Cardiac catheterization, especially if the procedure involves blood vessels in the groin
- Certain medications, including some blood thinners (anticoagulants) and medications used to control bleeding (antifibrinolytics)
- High blood pressure
- Increased body mass index (BMI)
Complications
Left untreated, an arteriovenous fistula can cause complications. Some complications may be serious. These include:
- Heart failure. This is the most serious complication of large arteriovenous fistulas. Blood flows more quickly through an arteriovenous fistula than it does through typical blood vessels. The increased blood flow makes the heart pump harder. Over time, the strain on the heart can lead to heart failure.
- Blood clots. An arteriovenous fistula in the legs can cause blood clots to form. Leg blood clots may lead to a condition called deep vein thrombosis (DVT). DVT can be life-threatening if the clot travels to the lungs (pulmonary embolism). Depending on where the fistula is, it may lead to a stroke.
- Leg pain due to lack of blood flow (claudication). An arteriovenous fistula can block blood flow to muscles, causing leg pain.
- Internal bleeding. Arteriovenous fistulas may cause bleeding in the stomach and intestines.
Diagnosis
To diagnose an arteriovenous fistula, a health care provider may use a stethoscope to listen to the blood flow in the arms and legs. The blood flow through an arteriovenous fistula makes a sound like humming.
If your provider thinks you have a fistula, other tests are typically done to confirm the diagnosis. Tests to diagnose an arteriovenous fistula can include:
- Duplex ultrasound. Duplex ultrasound is the most effective and common way to check for an arteriovenous fistula in the legs or arms. In duplex ultrasound, sound waves are used to evaluate the speed of blood flow.
- Computerized tomography (CT) angiogram. This imaging test can show if blood flow is bypassing the capillaries. Dye (contrast) is given by IV for this test. The dye helps blood vessels show up more clearly on the images.
- Magnetic resonance angiography (MRA). This test may be done if you have signs of an arteriovenous fistula deep under the skin. Like an MRI, an MRA uses a magnetic field and radio waves to create pictures of the body's soft tissues. Dye (contrast) is given by IV to help blood vessels show up better on the images.
Treatment
If an arteriovenous fistula is small and doesn't cause any other health problems, close monitoring by a health care provider may be the only treatment needed. Some small arteriovenous fistulas close by themselves without treatment.
If an arteriovenous fistula requires treatment, your provider may recommend:
- Ultrasound-guided compression. This may be an option for an arteriovenous fistula in the legs that's easily seen on ultrasound. In this treatment, an ultrasound probe is push down on the fistula for about 10 minutes. The compression destroys blood flow to the damaged blood vessels.
- Catheter embolization. In this procedure, a thin, flexible tube (catheter) is inserted in an artery near the arteriovenous fistula. Then, a small coil or stent is placed at the site of the fistula to reroute blood flow. Many people who have catheter embolization stay in the hospital for less than a day and can resume daily activities within a week.
- Surgery. Large arteriovenous fistulas that can't be treated with catheter embolization may require surgery. The type of surgery needed depends on the size and location of the arteriovenous fistula.
Preparing for your appointment
If you think you may have an arteriovenous fistula, make an appointment with your primary care provider. You may be referred to a doctor trained in blood vessel (vascular) or heart (cardiologist) diseases.
Appointments can be brief. Because there's often a lot of ground to cover, it's a good idea to be prepared for your appointment. Here's some information to help you get ready for your appointment and know what to expect from your provider.
What you can do
- Write down any symptoms you're having, including any that may seem unrelated to an arteriovenous fistula.
- Write down key personal information, including previous piercing injuries or a family history of arteriovenous fistulas or other blood vessel diseases.
- Make a list of all medications, vitamins or supplements that you're taking. Include their doses.
- Take a family member or friend along, if possible. Sometimes it can be difficult to recall all the information provided to you during an appointment. Someone who goes with you may remember something that you missed or forgot.
- Write down questions to ask your health care provider.
For an arteriovenous fistula, some basic questions to ask include:
- What's the most likely cause of my symptoms?
- Are there any other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatments are available, and which do you recommend?
- What's an appropriate level of physical activity?
- I have other health conditions. How can I best manage these conditions together?
- Should my children or other biological relatives be screened for this condition?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
What to expect from your doctor
Your health care provider is likely to ask you many questions. Being ready to answer them may save time to go over any details you want to spend more time on. Your provider may ask:
- When did you first begin having symptoms?
- Do you always have symptoms, or do they come and go?
- How severe are the symptoms?
- Does anything seem to improve the symptoms?
- What, if anything, makes symptoms worse?
Last Updated May 17, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use