Cataracts
Overview
A cataract is a clouding of the lens of the eye, which is typically clear. For people who have cataracts, seeing through cloudy lenses is like looking through a frosty or fogged-up window. Clouded vision caused by cataracts can make it more difficult to read, drive a car at night or see the expression on a friend's face.
Most cataracts develop slowly and don't disturb eyesight early on. But with time, cataracts will eventually affect vision.
At first, stronger lighting and eyeglasses can help deal with cataracts. But if impaired vision affects usual activities, cataract surgery might be needed. Fortunately, cataract surgery is generally a safe, effective procedure.

A cataract occurs when the lens of your eye becomes cloudy. Eventually, a cataract can become like the one shown in this person's right eye.

Clear vision, like on the left, becomes blurred as a cataract forms, like on the right.
Symptoms
Symptoms of cataracts include:
- Clouded, blurred or dim vision.
- Trouble seeing at night.
- Sensitivity to light and glare.
- Need for brighter light for reading and other activities.
- Seeing "halos" around lights.
- Frequent changes in eyeglass or contact lens prescription.
- Fading or yellowing of colors.
- Double vision in one eye.
At first, the cloudiness in your vision caused by a cataract may affect only a small part of the eye's lens. You may not notice any vision loss. As the cataract grows larger, it clouds more of your lens. More clouding changes the light passing through the lens. This may lead to symptoms you notice more.
When to see a doctor
Make an appointment for an eye exam if you notice any changes in your vision. If you develop sudden vision changes, such as double vision or flashes of light, sudden eye pain, or a sudden headache, see a member of your health care team right away.
Causes
Most cataracts develop when aging or injury changes the tissue that makes up the eye's lens. Proteins and fibers in the lens begin to break down. This causes vision to become hazy or cloudy.
Some disorders passed down from parents that cause other health problems can increase your risk of cataracts. Cataracts also can be caused by other eye conditions, past eye surgery or medical conditions such as diabetes. Long-term use of steroid medicines also may cause cataracts to develop.
How a cataract forms
A cataract is a cloudy lens. The lens sits behind the colored part of your eye, called the iris. The lens focuses light that passes into your eye. This produces clear, sharp images on the back part of the eye, called the retina.
As you age, the lenses in your eyes become less flexible, less clear and thicker. Aging and some medical conditions can cause proteins and fibers within the lenses to break down and clump together. This is what causes the clouding in the lenses.
As the cataract grows, the clouding becomes worse. A cataract scatters and blocks the light as it passes through the lens. This prevents a sharply defined image from reaching your retina. As a result, your vision becomes blurred.
Cataracts usually happen in both eyes, but not always at the same rate. The cataract in one eye may be worse than the other. This causes a difference in vision between eyes.
Types of cataracts
Cataract types include:
- Cataracts affecting the center of the lens, called nuclear cataracts. A nuclear cataract may at first cause objects far away to be blurry but objects up close to look clear. A nuclear cataract may even improve your reading vision for a short time. But with time, the lens slowly turns more yellow or brown and makes your vision worse. It may become difficult to tell colors apart.
- Cataracts that affect the edges of the lens, called cortical cataracts. A cortical cataract begins as white, wedge-shaped spots or streaks on the outer edge of the lens cortex. As the cataract slowly grows, the streaks spread to the center and affect light passing through the lens.
- Cataracts that affect the back of the lens, called posterior subcapsular cataracts. A posterior subcapsular cataract starts as a small spot that usually forms near the back of the lens, right in the path of light. A posterior subcapsular cataract often affects your reading vision. It also may reduce your vision in bright light and cause glare or halos around lights at night. These types of cataracts tend to grow faster than others.
-
Cataracts you're born with, called congenital cataracts. Some people are born with cataracts or develop them during childhood. These cataracts may be passed down from parents. They also may be associated with an infection or trauma while in the womb.
These cataracts also may be due to certain conditions. These may include myotonic dystrophy, galactosemia, neurofibromatosis type 2 or rubella. Congenital cataracts don't always affect vision. If they do, they're usually removed soon after they're found.
Risk factors
Factors that increase your risk of cataracts include:
- Increasing age.
- Diabetes.
- Getting too much sunlight.
- Smoking.
- Obesity.
- Family history of cataracts.
- Previous eye injury or inflammation.
- Previous eye surgery.
- Prolonged use of corticosteroid medicines.
- Drinking excessive amounts of alcohol.
Prevention
No studies have proved how to prevent or slow the growth of cataracts. But health care professionals think several strategies may be helpful, including:
- Regular eye exams. Eye exams can help detect cataracts and other eye problems at their earliest stages. Ask your health care team how often you should have an eye examination.
- Do not smoke. Ask a member of your health care team how to stop smoking. Medicines, counseling and other strategies are available to help you.
- Manage other health problems. Follow your treatment plan if you have diabetes or other medical conditions that can increase your risk of cataracts.
-
Choose a healthy diet that includes plenty of fruits and vegetables. Adding fruits and vegetables to your diet ensures that you're getting many vitamins and nutrients. Fruits and vegetables have antioxidants. Antioxidants help maintain the health of your eyes.
Studies haven't proved that antioxidants in pill form can prevent cataracts. But a large population study recently showed that a healthy diet rich in vitamins and minerals reduced the risk of developing cataracts. Fruits and vegetables have many proven health benefits. Eating them is a safe way to get enough minerals and vitamins in your diet.
- Wear sunglasses. Ultraviolet light from the sun may cause cataracts. Wear sunglasses that block ultraviolet B rays when you're outdoors.
- Reduce alcohol use. Drinking too much alcohol can increase the risk of cataracts.
Diagnosis
To determine whether you have a cataract, your eye doctor will review your medical history and symptoms. They also will perform an eye exam. Your doctor may do several tests, including:
- Vision test. A vision test, also called a visual acuity test, uses an eye chart to measure how well you can read a series of letters. One eye is tested at a time, while the other eye is covered. A chart or a viewing device with letters that get smaller is used. With this, your eye doctor determines if you have 20/20 vision or if you have trouble seeing.
- Eye structure exam. An eye structure exam, also called a slit lamp, allows your eye doctor to see the structures at the front of your eye up close. It's called a slit lamp because it uses an intense line of light, a slit, to light up the structures in your eye. The slit allows your doctor to view these structures in small sections. This makes it easier to find anything that may be wrong.
- Retinal exam. A retinal exam looks at the back of your eyes, called the retina. To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide, called dilation. This makes it easier to see the retina. Using a slit lamp or a special device called an ophthalmoscope, your eye doctor can examine your lens for signs of a cataract.
- Fluid pressure test. This test, also called applanation tonometry, measures fluid pressure in your eye. There are multiple different devices available to do this.
Treatment
When your prescription glasses can't clear your vision, the only effective treatment for cataracts is surgery.
When to consider cataract surgery
Talk with your eye doctor about whether surgery is right for you. Most eye doctors suggest considering cataract surgery when your cataracts begin to affect your quality of life. This may include your ability to perform daily activities, such as reading or driving at night.
For most people, there is no rush to remove cataracts because they usually don't harm the eyes. But cataracts can worsen faster in people with certain conditions. These include diabetes, high blood pressure or obesity.
Waiting to do cataract surgery typically won't affect how well your vision recovers. Take time to consider the benefits and risks of cataract surgery with your doctor.
If you choose not to have cataract surgery now, your eye doctor may recommend periodic follow-up exams to see if your cataracts are getting worse. How often you'll see your eye doctor depends on your situation.
What happens during cataract surgery
Cataract surgery involves removing the clouded lens and replacing it with a clear artificial lens. The artificial lens, called an intraocular lens, is put in the same place as your natural lens. It remains a permanent part of your eye.
For some people, artificial lenses can't be used. In these situations, once the cataract is removed, vision may be corrected with eyeglasses or contact lenses.
Cataract surgery is typically done on an outpatient basis. This means you won't need to stay in a hospital after the surgery. During surgery, your eye doctor uses a medicine to numb the area around your eye. You usually stay awake during the procedure.
Cataract surgery is generally safe. However, it carries a risk of infection and bleeding. Cataract surgery also increases the risk of the retina being pulled out of place. This is called retinal detachment.
After the procedure, you may be sore for a few days. Healing usually happens within a few weeks.
If you need cataract surgery in both eyes, your doctor will schedule surgery to remove the cataract in the second eye after you've healed from the first surgery.
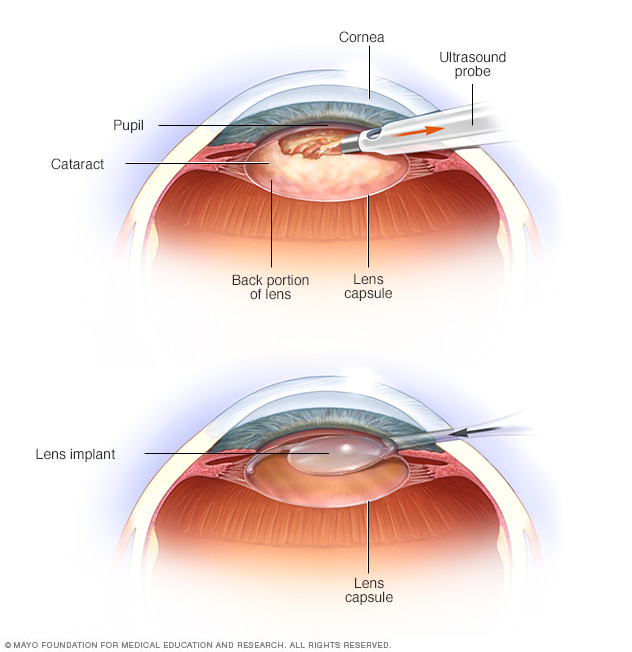
The most common type of cataract surgery is called phacoemulsification. During this process, the rapidly vibrating tip of an ultrasound probe breaks up the cataract. Your surgeon then suctions out the lens, as seen in the top image. An outer housing of the cataract, called the lens capsule, is generally left in place. After removing the lens, your surgeon places the lens implant into the empty space within the capsule where the natural lens used to be, as seen in the bottom image.
Lifestyle and home remedies
To deal with symptoms of cataracts until you decide to have surgery, try to:
- Make sure your prescription for your eyeglasses or contact lenses is up to date.
- Use a magnifying glass to read if you need more help reading.
- Improve the lighting in your home with more or brighter lamps.
- Wear sunglasses or a broad-brimmed hat to reduce glare during the day.
- Limit driving at night.
Self-care measures may help for a while, but your vision may get worse as the cataract grows. When vision loss starts to affect your everyday activities, consider cataract surgery.
Preparing for an appointment
Make an appointment with your usual eye care professional if you notice changes in your vision. If they determine that you have cataracts, then you may be referred to an eye specialist who can perform cataract surgery.
There's often a lot to talk about. It's a good idea to be well prepared for your appointment so that you can make the most of your time. Here's some information to help you get ready.
What you can do
- List any symptoms you're experiencing, including any that may not seem related to the reason you scheduled the appointment.
- Make a list of all medicines, vitamins or supplements that you're taking.
- Take a family member or friend along. Sometimes it can be difficult to absorb all the information provided during an appointment. Someone who comes with you may remember something that you missed or forgot.
- List questions to ask your health care team.
For cataracts, some basic questions to ask include:
- Are cataracts causing my vision problems?
- What kinds of tests do I need?
- Will cataract surgery correct my vision problems?
- What are the potential risks of cataract surgery? Are there risks in waiting to do surgery?
- What will cataract surgery cost, and will my insurance cover it?
- How much time will I need to recover from cataract surgery?
- Will any usual activities be restricted after cataract surgery? For how long?
- After cataract surgery, how long should I wait before getting new glasses?
- If I use Medicare, will it cover the cost of cataract surgery? Does Medicare cover the cost of new glasses after surgery?
- If I don't want surgery right now, what else can I do to help with my vision changes?
- How will I know if my cataracts are getting worse?
- I have these other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared, don't hesitate to ask questions at any time if you don't understand something.
What to expect from your doctor
Your health care team is likely to ask you a number of questions. Being ready to answer them may allow more time later to cover other points you want to address. You may be asked:
- When did you begin having symptoms?
- Do you have your symptoms all the time or do they come and go?
- Do you have vision problems in bright light?
- Have your symptoms gotten worse?
- Do your vision problems make it difficult for you to drive?
- Do your vision problems make it difficult to read?
- Do your vision problems make it difficult to do your job?
- Have you ever had an eye injury or eye surgery?
- Have you ever been diagnosed with an eye problem, such as inflammation of your iris?
- Have you ever received radiation therapy to your head or neck?
Last Updated Sep 28, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use