Cervicitis
Overview
Cervicitis is an inflammation of the cervix, the lower, narrow end of the uterus that opens into the vagina.
Possible symptoms of cervicitis include bleeding between menstrual periods, pain with intercourse or during a pelvic exam, and abnormal vaginal discharge. However, it's also possible to have cervicitis and not experience any signs or symptoms.
Often, cervicitis results from a sexually transmitted infection, such as chlamydia or gonorrhea. Cervicitis can develop from noninfectious causes, too. Successful treatment of cervicitis involves treating the underlying cause of the inflammation.
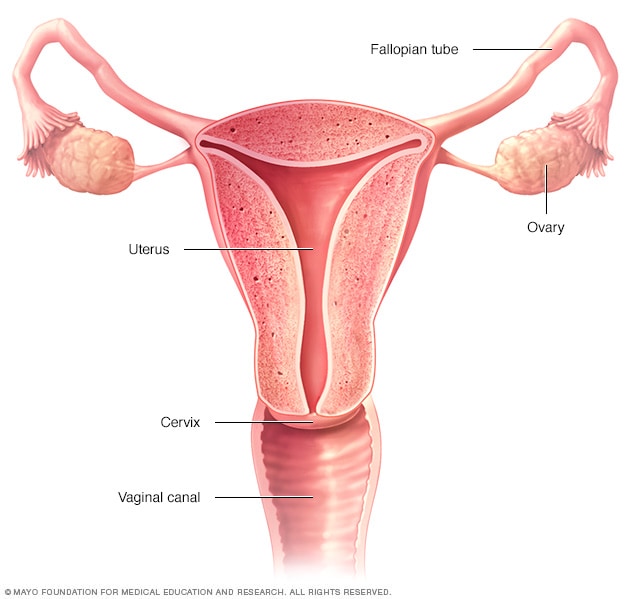
The ovaries, fallopian tubes, uterus, cervix and vagina (vaginal canal) make up the female reproductive system.
Symptoms
Most often, cervicitis causes no signs and symptoms, and you may only learn you have the condition after a pelvic exam performed by your doctor for another reason. If you do have signs and symptoms, they may include:
- Large amounts of unusual vaginal discharge
- Frequent, painful urination
- Pain during sex
- Bleeding between menstrual periods
- Vaginal bleeding after sex, not associated with a menstrual period
When to see a doctor
See your doctor if you have:
- Persistent, unusual vaginal discharge
- Nonmenstrual vaginal bleeding
- Pain during sex
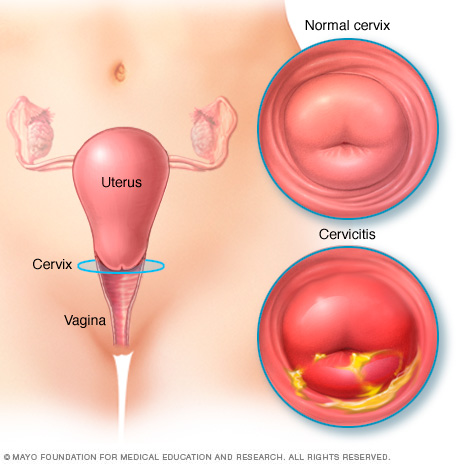
With cervicitis, an inflammation of your cervix, your cervix appears red and irritated and may produce a pus-like discharge.
Causes
Possible causes of cervicitis include:
- Sexually transmitted infections. Most often, the bacterial and viral infections that cause cervicitis are transmitted by sexual contact. Cervicitis can result from common sexually transmitted infections (STIs), including gonorrhea, chlamydia, trichomoniasis and genital herpes.
- Allergic reactions. An allergy, either to contraceptive spermicides or to latex in condoms, may lead to cervicitis. A reaction to feminine hygiene products, such as douches or feminine deodorants, also can cause cervicitis.
- Bacterial overgrowth. An overgrowth of some of the bacteria that are normally present in the vagina (bacterial vaginosis) can lead to cervicitis.
Risk factors
You're at greater risk of cervicitis if you:
- Engage in high-risk sexual behavior, such as unprotected sex, sex with multiple partners or sex with someone who engages in high-risk behaviors
- Began having sexual intercourse at an early age
- Have a history of sexually transmitted infections
Complications
Your cervix acts as a barrier to keep bacteria and viruses from entering your uterus. When the cervix is infected, there's an increased risk that the infection will travel into your uterus.
Cervicitis that's caused by gonorrhea or chlamydia can spread to the uterine lining and the fallopian tubes, resulting in pelvic inflammatory disease (PID), an infection of the female reproductive organs that can cause fertility problems if left untreated.
Cervicitis can also increase the risk of getting HIV from an infected sexual partner.
Prevention
To reduce your risk of cervicitis from sexually transmitted infections, use condoms consistently and correctly each time you have sex. Condoms are very effective against the spread of STIs, such as gonorrhea and chlamydia, which can lead to cervicitis. Being in a long-term relationship in which both you and your uninfected partner are committed to having sex with each other exclusively can lower your odds of an STI.
Diagnosis
To diagnose cervicitis, your doctor will likely perform a physical exam that includes:
- A pelvic exam. During this exam, your doctor checks your pelvic organs for areas of swelling and tenderness. He or she may also place a speculum in your vagina to view the upper, lower and side walls of the vagina and the cervix.
- A specimen collection. In a process similar to a Pap test, your doctor uses a small cotton swab or a brush to gently remove a sample of cervical and vaginal fluid. Your doctor sends the sample to a lab to test for infections. Lab tests may also be performed on a urine sample.
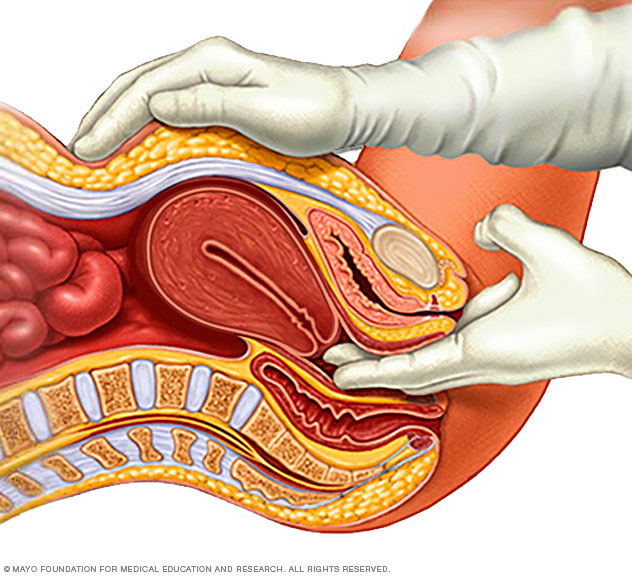
During a pelvic exam, a doctor inserts one or two gloved fingers inside the vagina. Pressing down on the abdomen at the same time, the doctor can check the uterus, ovaries and other organs.
Treatment
You won't need treatment for cervicitis caused by an allergic reaction to products such as spermicide or feminine hygiene products. If you have cervicitis caused by a sexually transmitted infection (STI), both you and your partner will need treatment, often with an antibiotic medication. Antibiotics are prescribed for STIs such as gonorrhea, chlamydia or bacterial infections, including bacterial vaginosis.
Your doctor may offer antiviral medication if you have genital herpes, which helps decrease the amount of time you have cervicitis symptoms. However, there is no cure for herpes. Herpes is a chronic condition that may be passed to your sexual partner at any time.
Your doctor may also recommend repeat testing for cervicitis caused by gonorrhea or chlamydia.
To avoid passing a bacterial infection along to your partner, wait to have sex until you're finished with the treatment recommended by your doctor.
Preparing for an appointment
Cervicitis may be discovered incidentally during a routine pelvic exam and may not require treatment if it's not due to an infection. If, however, you experience unusual vaginal symptoms that lead you to schedule an appointment, you'll most likely see a gynecologist or primary care doctor.
Here's some information to help you get ready for your appointment.
What you can do
- Avoid using tampons.
- Don't douche.
- Know the name of your partner, and the dates you had sexual relations.
- Make a list of all medications or supplements you're taking.
- Know your allergies.
- Write down questions you have.
Some basic questions include:
- How did I get this condition?
- Do I need to take medicine?
- Are there any over-the-counter products that will treat my condition?
- Does my partner also need to be tested or treated?
- What should I do if my symptoms return after treatment?
- What can I do to prevent cervicitis in the future?
Don't hesitate to ask additional questions during your appointment if you think of something else.
What to expect from your doctor
Your doctor will likely perform a physical exam that may include a pelvic exam and Pap test. He or she may collect a fluid specimen from your vagina or cervix to send for testing.
Your doctor may also ask you a number of questions about your condition, such as:
- What vaginal symptoms are you experiencing?
- Are you experiencing any urinary problems, such as pain during urination?
- How long have you had your symptoms?
- Are you sexually active?
- Have you or your partner ever had a sexually transmitted infection?
- Do you experience pain or bleeding during sex?
- Do you douche or use any feminine hygiene products?
- Are you pregnant?
- Have you tried any over-the-counter products to treat your symptoms?
Last Updated Jan 31, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use