Chondrosarcoma
Overview
Chondrosarcoma is a rare type of cancer that usually begins in the bones, but can sometimes occur in the soft tissue near bones. Chondrosarcoma happens most often in the pelvis, hip and shoulder. More rarely, it can happen in the bones of the spine.
Most chondrosarcomas grow slowly and may not cause many signs and symptoms at first. Some rare types grow rapidly and have a high risk of spreading to other areas of the body, which can make these cancers difficult to treat.
Chondrosarcoma treatment usually involves surgery. Other options might include radiation therapy and chemotherapy.
Symptoms
Chondrosarcoma tends to grow slowly, so it might not cause signs and symptoms at first. When they occur, signs and symptoms of chondrosarcoma may include:
- Increasing pain
- A growing lump or area of swelling
- Weakness or bowel and bladder control problems, if the cancer presses on the spinal cord
Causes
It's not clear what causes chondrosarcoma. Doctors know that cancer begins when a cell develops changes (mutations) in its DNA. A cell's DNA contains the instructions that tell it what to do. The instructions tell the cell to multiply quickly and to continue living when healthy cells would die. The accumulating cells form a tumor that can grow to invade and destroy normal body tissue. In time, cells can break away and spread (metastasize) to other areas of the body.
Risk factors
Factors that can increase the risk of chondrosarcoma include:
- Increasing age. Chondrosarcoma occurs most often in middle-aged and older adults, though it can occur at any age.
- Other bone diseases. Ollier's disease and Maffucci's syndrome are conditions that cause noncancerous bone growths (enchondromas) in the body. These growths sometimes transform into chondrosarcoma.
Diagnosis
Tests and procedures used to diagnose chondrosarcoma include:
- Physical exam. Your doctor may ask about your signs and symptoms and examine your body to gather more clues about your diagnosis.
- Imaging tests. Imaging tests may include X-ray, bone scan, MRI and CT scan.
-
Removing a sample of tissue for testing (biopsy). Biopsy is a procedure to collect suspicious tissue. The tissue is sent to a lab where doctors analyze it to determine whether it's cancer.
How the biopsy sample is collected depends on where the suspicious tissue is located. The procedure requires careful planning so that the biopsy is done in a way that won't interfere with future surgery to remove the cancer. For this reason, ask your doctor for a referral to a team of experts with experience in treating chondrosarcoma.
Treatment
Chondrosarcoma treatment often involves surgery to remove the cancer. Other treatments might be recommended in certain situations. Which options are best for you depends on where your cancer is located, how quickly it's growing, whether it has grown to involve other structures, your overall health and your preferences.
Surgery
The goal of surgery for chondrosarcoma is to remove the cancer and a margin of healthy tissue around it. The type of surgery you undergo will depend on the location of your chondrosarcoma. Options might include:
- Scraping the cancer away from the bone. Small and slow-growing chondrosarcomas in the arms and legs are sometimes treated with a procedure to scrape the cancer cells from the bone. The surgeon might apply cold gas or a chemical to kill any cancer cells that remain. The bone can be repaired with a bone graft or bone cement, if needed.
- Cutting away the cancer and some healthy tissue around it. Most chondrosarcomas require a procedure to cut away more of the bone in order to remove all of the cancer. For chondrosarcoma in an arm or a leg, it might be necessary to remove the entire limb. When possible, surgeons remove the cancer in a way that preserves the limb. For example, the surgeon might remove the affected bone and replace it or reconstruct it (limb salvage surgery).
Radiation therapy
Radiation therapy uses high-powered energy beams from sources such as X-rays and protons to kill cancer cells. During radiation therapy, you lie on a table while a machine moves around you, directing radiation to precise points on your body.
Radiation might be recommended for chondrosarcomas located in places that make surgery tricky or if the cancer can't be removed completely during surgery. Radiation may also be used to control cancer that spreads to other areas of the body.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. It's not often used for chondrosarcoma because this type of cancer often doesn't respond to chemotherapy. But some fast-growing types of chondrosarcoma may respond to this treatment.
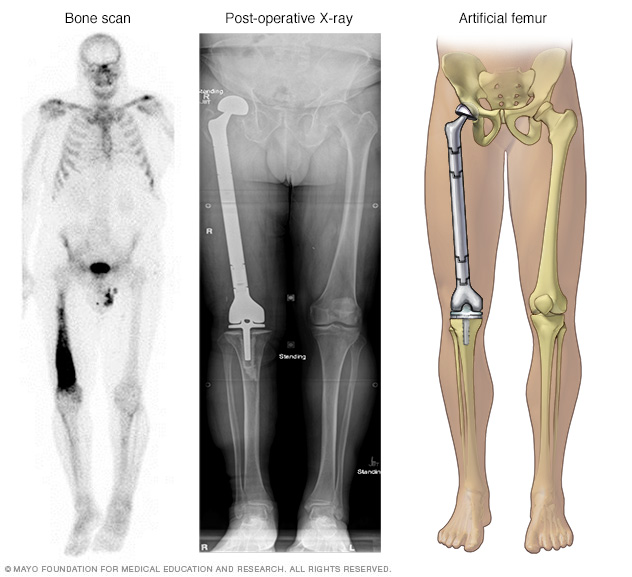
A bone scan (left) shows cancer in right thighbone, also called the femur. The entire thighbone, plus the hip joint and knee joint, were replaced with artificial components.
Coping and support
A cancer diagnosis can change your life forever. Each person finds his or her own way of coping with the emotional and physical changes cancer brings. But when you're first diagnosed with cancer, sometimes it's difficult to know what to do next.
Here are some ideas to help you cope:
- Learn enough about cancer to make decisions about your care. Ask your doctor about your cancer, including your treatment options and, if you like, your prognosis. As you learn more about cancer, you may become more confident in making treatment decisions.
- Keep friends and family close. Keeping your close relationships strong will help you deal with your cancer. Friends and family can provide the practical support you'll need, such as helping take care of your home if you're in the hospital. And they can serve as emotional support when you feel overwhelmed by cancer.
- Find someone to talk with. Find a good listener who is willing to listen to you talk about your hopes and fears. This may be a friend or family member. The concern and understanding of a counselor, medical social worker, clergy member or cancer support group also may be helpful.
Preparing for an appointment
Start by seeing your family doctor if you have any signs or symptoms that worry you. If your doctor determines you have cancer, you'll likely be referred to one or more specialists, such as doctors who treat cancer (oncologists) and surgeons.
What you can do
- Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
- Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
- Write down key personal information, including any major stresses or recent life changes.
- Write down your family's history of cancer. If other members of your family have been diagnosed with cancer, make a note of the types of cancer, how each person is related to you and how old each person was when diagnosed.
- Make a list of all medications, vitamins or supplements that you're taking.
- Consider taking a family member or friend along. Sometimes it can be difficult to remember all the information provided during an appointment. Someone who accompanies you may remember something that you missed or forgot.
- Write down questions to ask your doctor.
Preparing a list of questions in advance can help you make the most of your time with your doctor. List your questions from most important to least important in case time runs out. For cancer, some basic questions to ask your doctor include:
- What type of cancer do I have?
- Will I need additional tests?
- What are my treatment options?
- Can treatments cure my cancer?
- If my cancer can't be cured, what can I expect from treatment?
- What are the potential side effects of each treatment?
- Is there one treatment you feel is best for me?
- How soon do I need to begin treatment?
- How will treatment affect my daily life?
- Can I continue working during treatment?
- Are there any clinical trials or experimental treatments available to me?
- I have these other health conditions. How can I manage them during my cancer treatment?
- Are there any restrictions that I need to follow?
- Should I see a specialist? What will that cost, and will my insurance cover it?
- Is there a generic alternative to the medicine you're prescribing?
- Are there brochures or other printed material that I can take with me? What websites do you recommend?
- What will determine whether I should plan for follow-up visits?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your doctor may ask:
- When did you first begin experiencing symptoms?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Does anyone in your family have cancer?
- Have you ever had cancer before? If so, what kind and how was it treated?
Last Updated Dec 7, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use