Deep vein thrombosis (DVT)
Overview
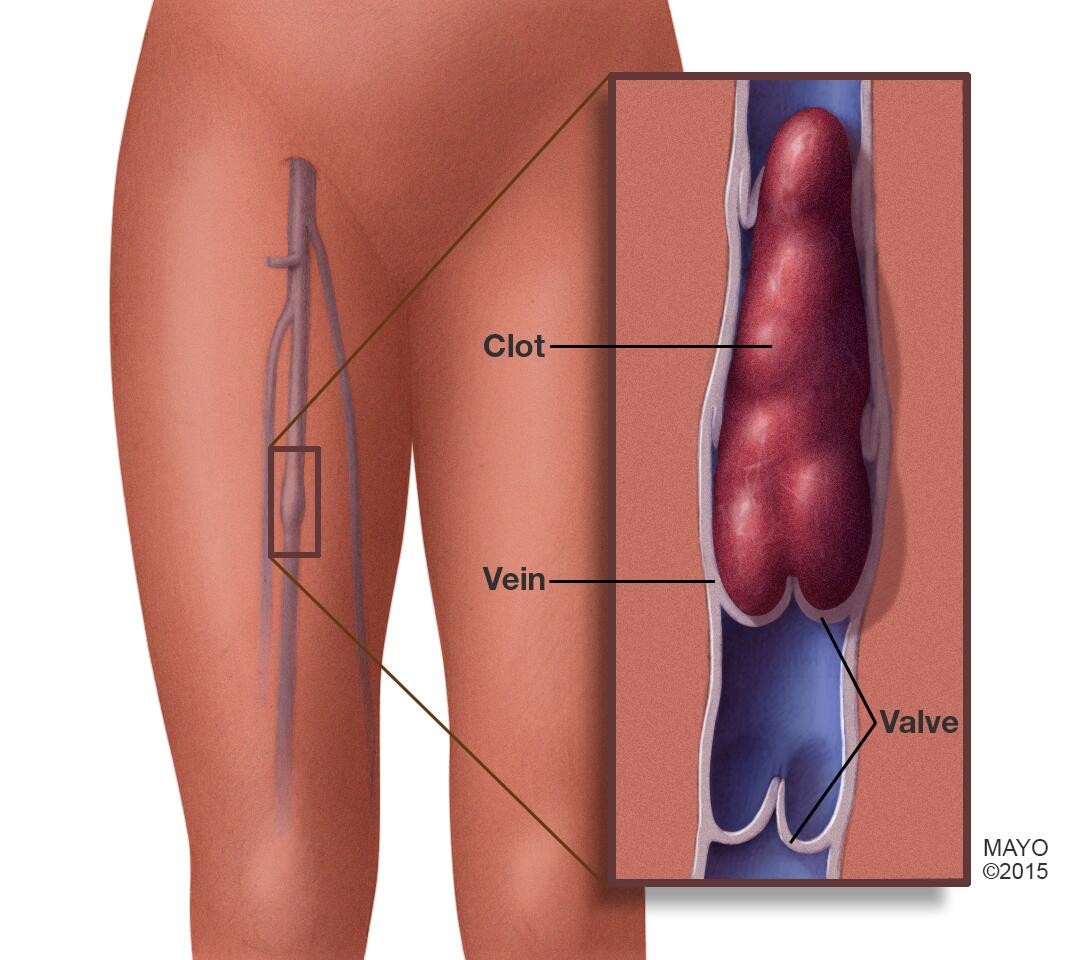
Deep vein thrombosis (DVT) occurs when a blood clot (thrombus) forms in one or more of the deep veins in the body, usually in the legs. Deep vein thrombosis can cause leg pain or swelling. Sometimes there are no noticeable symptoms.
You can get DVT if you have certain medical conditions that affect how the blood clots. A blood clot in the legs can also develop if you don't move for a long time. For example, you might not move a lot when traveling a long distance or when you're on bed rest due to surgery, an illness or an accident.
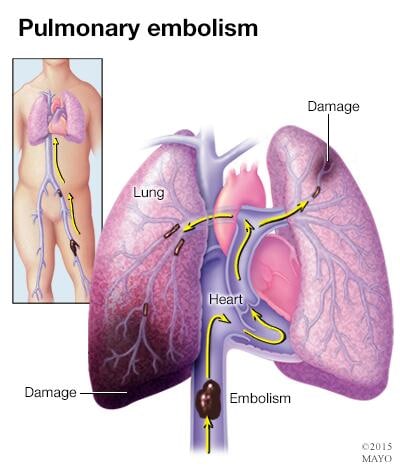
Deep vein thrombosis can be serious because blood clots in the veins can break loose. The clots can then travel through the bloodstream and get stuck in the lungs, blocking blood flow (pulmonary embolism). When DVT and pulmonary embolism occur together, it's called venous thromboembolism (VTE).
Symptoms
Deep vein thrombosis (DVT) symptoms can include:
- Leg swelling
- Leg pain, cramping or soreness that often starts in the calf
- Change in skin color on the leg — such as red or purple, depending on the color of your skin
- A feeling of warmth on the affected leg
Deep vein thrombosis can occur without noticeable symptoms.
When to see a doctor
If you develop symptoms of DVT, contact your health care provider.
If you develop symptoms of a pulmonary embolism (PE) — a life-threatening complication of deep vein thrombosis — seek emergency medical help.
The warning signs and symptoms of a pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens when you take a deep breath or when you cough
- Feeling lightheaded or dizzy
- Fainting
- Rapid pulse
- Rapid breathing
- Coughing up blood
Causes
Anything that prevents the blood from flowing or properly clotting can cause a blood clot.
The main causes of deep vein thrombosis (DVT) are damage to a vein from surgery or inflammation and damage due to infection or injury.
Risk factors
Many things can increase the risk of developing deep vein thrombosis (DVT). The more risk factors you have, the greater your risk of DVT. Risk factors for DVT include:
- Age. Being older than 60 increases the risk of DVT. But DVT can occur at any age.
- Lack of movement. When the legs don't move for a long time, the calf muscles don't squeeze (contract). Muscle contractions help blood flow. Sitting for a long time, such as when driving or flying, increases the risk of DVT. So does long-term bed rest, which may result from a lengthy hospital stay or a medical condition such as paralysis.
- Injury or surgery. Injury to the veins or surgery can increase the risk of blood clots.
- Pregnancy. Pregnancy increases the pressure in the veins in the pelvis and legs. The risk of blood clots from pregnancy can continue for up to six weeks after a baby is born. People with an inherited clotting disorder are especially at risk.
- Birth control pills (oral contraceptives) or hormone replacement therapy. Both can increase the blood's ability to clot.
- Being overweight or obese. Being overweight increases the pressure in the veins in the pelvis and legs.
- Smoking. Smoking affects how blood flows and clots, which can increase the risk of DVT.
- Cancer. Some cancers increase substances in the blood that cause the blood to clot. Some types of cancer treatment also increase the risk of blood clots.
- Heart failure. Heart failure increases the risk of DVT and pulmonary embolism. Because the heart and lungs don't work well in people with heart failure, the symptoms caused by even a small pulmonary embolism are more noticeable.
- Inflammatory bowel disease. Crohn's disease or ulcerative colitis increase the risk of DVT.
- A personal or family history of DVT or PE. If you or someone in your family has had one or both of these conditions, you might be at greater risk of developing DVT.
- Genetics. Some people have DNA changes that cause the blood to clot more easily. One example is factor V Leiden. This inherited disorder changes one of the clotting factors in the blood. An inherited disorder on its own might not cause blood clots unless combined with other risk factors.
Sometimes, a blood clot in a vein can occur with no identifiable risk factor. This is called an unprovoked VTE.
Complications
Complications of DVT can include:
-
Pulmonary embolism (PE). PE is a potentially life-threatening complication associated with DVT. It occurs when a blood clot (thrombus) in a leg or other body area breaks free and gets stuck in a blood vessel in a lung.
Get immediate medical help if you have symptoms of PE. They include sudden shortness of breath, chest pain while breathing in or coughing, rapid breathing, rapid pulse, feeling faint or fainting, and coughing up blood.
- Postphlebitic syndrome. Damage to the veins from the blood clot reduces blood flow in the affected areas. Symptoms include leg pain, leg swelling, skin color changes and skin sores.
- Treatment complications. Blood thinners are often used to treat DVT. Bleeding (hemorrhage) is a worrisome side effect of blood thinners. It's important to have regular blood tests while taking blood-thinning drugs.
Prevention
Lifestyle changes may help prevent deep vein thrombosis. Try these strategies:
-
Move your legs. If you've had surgery or have been on bed rest, try to move as soon as possible. Don't cross your legs while sitting. Doing so can block blood flow.
When traveling, take frequent breaks to stretch your legs. When on a plane, stand or walk occasionally. If you're traveling by car, stop every hour or so and walk around. If you can't walk, do lower leg exercises. Raise and lower your heels while keeping your toes on the floor. Then raise your toes while keeping your heels on the floor.
- Don't smoke. Smoking increases the risk of DVT.
- Manage weight. Obesity is a risk factor for DVT. Regular exercise lowers the risk of blood clots. As a general goal, aim for at least 30 minutes of moderate physical activity every day. If you want to lose weight, maintain weight loss or meet specific fitness goals, you may need to exercise more.
Diagnosis
To diagnose DVT, your health care provider will do a physical exam and ask questions about your symptoms. The provider will check the legs for swelling, tenderness or changes in skin color.
The tests you have depend on whether your provider thinks you are at a low or a high risk of DVT.
Tests
Tests used to diagnose or rule out DVT include:
- D-dimer blood test. D dimer is a type of protein produced by blood clots. Almost all people with severe DVT have increased blood levels of D dimer. This test often can help rule out PE.
- Duplex ultrasound. This noninvasive test uses sound waves to create pictures of how blood flows through the veins. It's the standard test for diagnosing DVT. For the test, a care provider gently moves a small hand-held device (transducer) on the skin over the body area being studied. Additional ultrasounds may be done over several days to check for new blood clots or to see if an existing one is growing.
- Venography. This test uses X-rays and dye to create a picture of the veins in the legs and feet. The dye is injected into a large vein in the foot or ankle. It helps blood vessels show up more clearly on X-rays. The test is invasive, so it's rarely done. Other tests, such as ultrasound, often are done first.
- Magnetic resonance imaging (MRI) scan. This test may be done to diagnose DVT in veins of the belly (abdomen).
Treatment
There are three main goals to DVT treatment.
- Prevent the clot from getting bigger.
- Prevent the clot from breaking loose and traveling to the lungs.
- Reduce the chances of another DVT.
DVT treatment options include:
-
Blood thinners. These medicines, also called anticoagulants, help prevent blood clots from getting bigger. Blood thinners reduce the risk of developing more clots.
Blood thinners may be taken by mouth or given by IV or an injection under the skin. There are many different types of blood-thinning drugs used to treat DVT. Together, you and your health care provider will discuss their benefits and risks to determine the best one for you.
You might need to take blood thinner pills for three months or longer. It's important to take them exactly as prescribed to prevent serious side effects.
People who take a blood thinner called warfarin (Jantoven) need regular blood tests to monitor levels of the drug in the body. Certain blood-thinning medications are not safe to take during pregnancy.
-
Clot busters (thrombolytics). These drugs are used for more-serious types of DVT or PE, or if other medications aren't working.
Clot busters are given by IV or through a tube (catheter) placed directly into the clot. They can cause serious bleeding, so they're usually only used for people with severe blood clots.
- Filters. If you can't take medicines to thin your blood, a filter may be placed into a large vein — the vena cava — in your belly (abdomen). A vena cava filter prevents clots that break loose from lodging in the lungs.
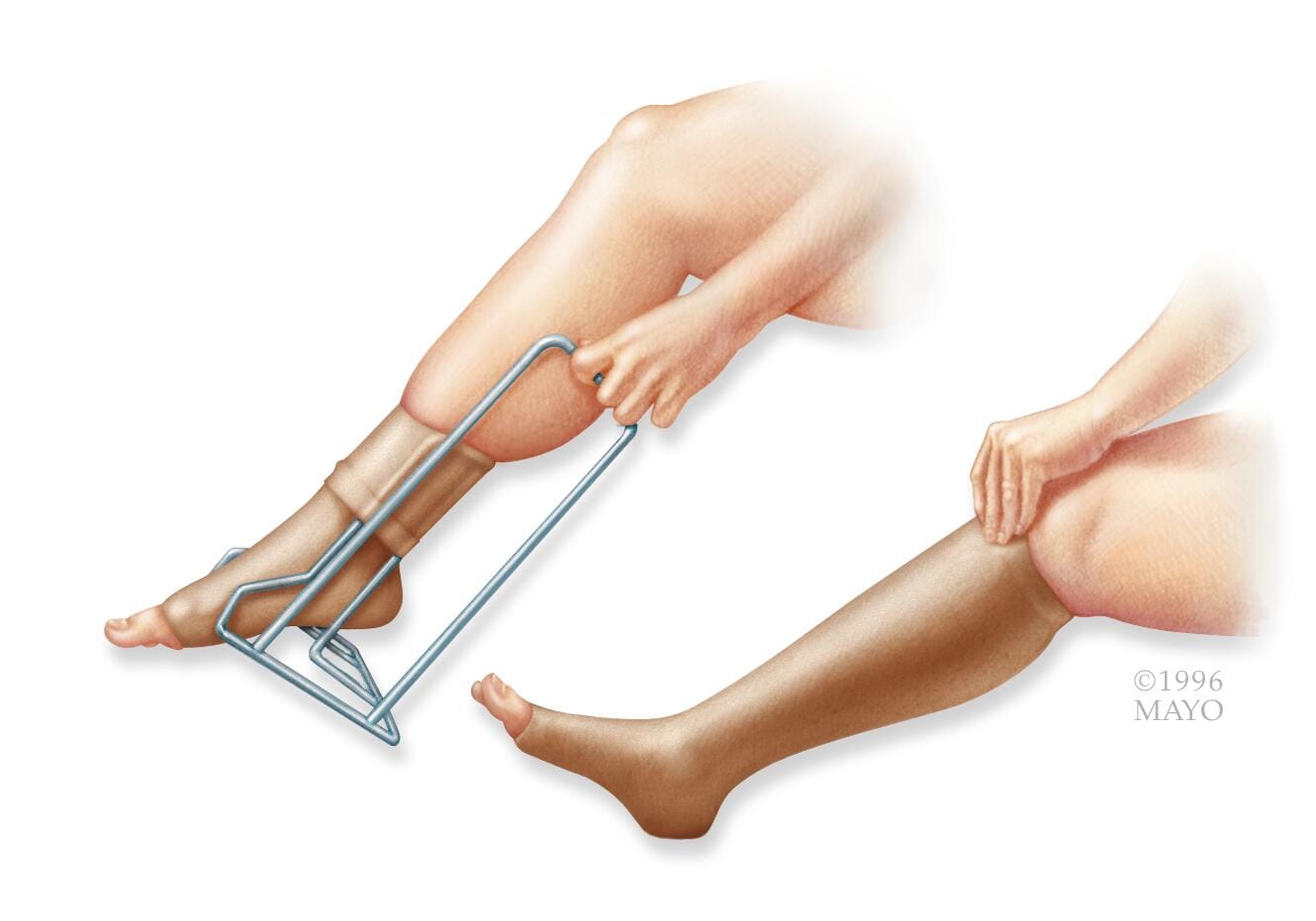
- Support stockings (compression stockings). These special knee socks help prevent blood from pooling in the legs. They help reduce leg swelling. Wear them on your legs from your feet to about the level of your knees. For DVT, you typically wear these stockings during the day for a few years, if possible.
Self care
After DVT treatment, follow these tips to manage the condition and prevent complications or more blood clots:
- Ask about your diet. Foods high in vitamin K, such as spinach, kale, other leafy greens and Brussels sprouts, can interfere with the blood thinner warfarin.
- Take medications as directed. Your provider will tell you how long you need treatment. If you're taking certain blood thinners, you'll need regular blood tests to see how well your blood is clotting.
- Watch for excessive bleeding. This can be a side effect of blood thinners. Ask your care provider about the warning signs. Know what to do if bleeding happens. Also ask your provider if you have activity restrictions. Minor injuries that cause bruising or even a simple cut may become serious if you're taking blood thinners.
- Move. If you've been on bed rest because of surgery or other reasons, the sooner you get moving, the lower the chance that blood clots will develop.
- Wear support stockings. Wear these to help prevent blood clots in the legs if your provider recommends them.
Preparing for your appointment
DVT is considered a medical emergency. It's important to get treated quickly. If there's time before your appointment, here's some information to help you get ready.
What you can do
Make a list of:
- Your symptoms, including any that seem unrelated to deep vein thrombosis, and when they began
- Important personal information, including notes about travel, hospital stays, any illness, surgery or trauma in the past three months, and any personal or family history of blood-clotting disorders
- All medications, vitamins or other supplements you take, including doses
- Questions to ask your health care provider
If possible, take a family member or friend with you to help you remember the information you're given.
For DVT, questions to ask your health care provider include:
- What's the most likely cause of my symptoms?
- What tests do I need?
- What's the best treatment?
- What are the options other than the main treatment that you're suggesting?
- Will I need to restrict travel or activities?
- I have other health conditions. How can I best manage these conditions together?
- Are there brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your health care provider is likely to ask you questions, such as:
- Have you been inactive lately, such as sitting or lying down for long periods?
- Do you always have symptoms, or do they come and go?
- How severe are your symptoms?
- What, if anything, makes your symptoms improve?
- What, if anything, makes your symptoms worse?
Last Updated Jun 11, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use