Esophagitis
Overview
Esophagitis (uh-sof-uh-JIE-tis) is inflammation of the esophagus. The esophagus is the muscular tube that delivers food from your mouth to your stomach.
Esophagitis can cause painful, difficult swallowing and chest pain. Many different things can cause esophagitis. Some common causes include stomach acids backing up into the esophagus, infection, oral medicines and allergies.
Treatment for esophagitis depends on the underlying cause and how badly the tissue lining the esophagus is damaged. If left untreated, esophagitis can damage this lining and interfere with its function, which is to move food and liquid from your mouth to your stomach. Esophagitis also can lead to complications such as scarring or narrowing of the esophagus, unintended weight loss and dehydration.
Symptoms
Common symptoms of esophagitis include:
- Difficulty swallowing.
- Painful swallowing.
- Swallowed food becoming stuck in the esophagus, also known as food impaction.
- Chest pain, particularly behind the breastbone, that occurs with eating.
- Heartburn.
- Acid regurgitation.
In infants and young children, particularly those too young to explain their discomfort or pain, symptoms of esophagitis may include:
- Feeding difficulties, such as irritability, arching of the back and not wanting to eat.
- Failure to thrive.
- Chest or belly pain in older children.
When to see a doctor
Most symptoms of esophagitis can be caused by a few different conditions affecting the digestive system. See your health care provider if symptoms:
- Last more than a few days.
- Aren't relieved by nonprescription antacids.
- Are bad enough to make eating difficult or if you are losing weight.
- Are accompanied by flu symptoms, such as headache, fever and muscle aches.
Get emergency care if you:
- Have pain in your chest that lasts more than a few minutes.
- Suspect you have food stuck in your esophagus.
- Have a history of heart disease and experience chest pain.
- Have pain in your mouth or throat when you eat.
- Have shortness of breath or chest pain that happens shortly after eating.
- Vomit large amounts, often have forceful vomiting, have trouble breathing after vomiting or have vomit that is yellow or green, looks like coffee grounds, or contains blood.
Causes
Esophagitis is generally labeled by the condition that causes it. In some cases, it may have more than one cause. Some of the most common types include:
Reflux esophagitis
A valve called the lower esophageal sphincter usually keeps the acidic contents of the stomach out of the esophagus. But sometimes this valve doesn't close properly or opens when it shouldn't. The upper part of the stomach can sometimes slide into the chest above the diaphragm, known as a hiatal hernia. If this happens, the contents of the stomach may back up into the esophagus (gastroesophageal reflux).
Gastroesophageal reflux disease (GERD) is a condition in which this backflow of acid is a frequent or ongoing problem. A complication of GERD is ongoing inflammation and tissue damage in the esophagus.
Eosinophilic esophagitis
Eosinophils (e-o-SIN-o-fils) are white blood cells that play a key role in allergic reactions. Eosinophilic esophagitis can occur if there is a high concentration of these white blood cells in the esophagus. This is most likely in response to an allergy-causing agent (allergen), acid reflux or both.
In many cases, this type of esophagitis may be triggered by foods such as milk, eggs, wheat, soy, peanuts and seafood. However, typical allergy testing does not reliably identify these culprit foods.
People with eosinophilic esophagitis may have other nonfood allergies. For example, sometimes allergens in the air, such as pollen, may be the cause. The most common symptom of eosinophilic esophagitis is food impaction or trouble swallowing, also called dysphagia.
Lymphocytic esophagitis
Lymphocytic esophagitis (LE) is an uncommon esophageal condition in which there are an increased number of white blood cells known as lymphocytes in the lining of the esophagus. LE may be related to eosinophilic esophagitis or to GERD.
Drug-induced esophagitis
Several oral medicines may cause tissue damage if they remain in contact with the lining of the esophagus for too long. For example, if you swallow a pill with little or no water, the pill itself or residue from the pill may remain in the esophagus. Medicines that have been linked to esophagitis include:
- Pain-relieving medications, such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve, others).
- Antibiotics, such as tetracycline and doxycycline.
- Potassium chloride, which is used to treat potassium deficiency.
- Bisphosphonates, including alendronate (Fosamax), a treatment for weak and brittle bones, called osteoporosis.
- Quinidine, which is used to treat heart problems.
Infectious esophagitis
A bacterial, viral or fungal infection in tissues of the esophagus may cause esophagitis. Infectious esophagitis is fairly rare and occurs most often in people with poor immune system function, such as people with HIV/AIDS or cancer.
A fungus usually present in the mouth called Candida albicans is a common cause of infectious esophagitis. Such infections are often associated with poor immune system function, diabetes, cancer, or the use of steroid or antibiotic medications.
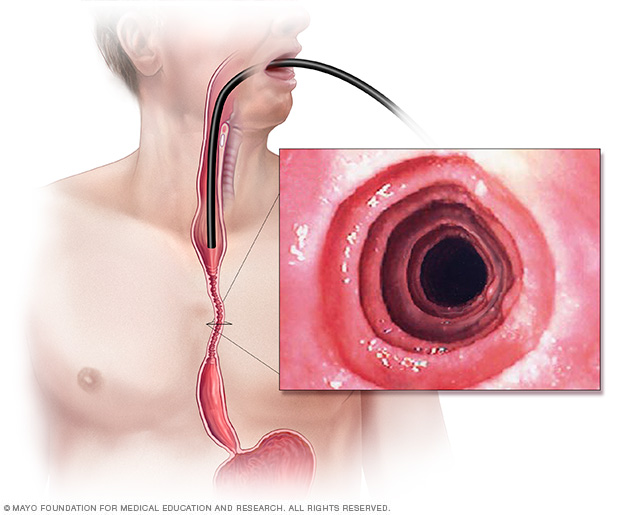
Esophagitis is inflammation that damages the lining of the esophagus. An endoscope — a long, flexible tube equipped with a camera — may be used to see inside your esophagus. This endoscopic image of eosinophilic esophagitis shows rings of irregular tissue resulting from chronic inflammation. These are known as esophageal rings.
Risk factors
Risk factors for esophagitis vary depending on the different causes of the disorder.
Reflux esophagitis
Factors that increase the risk of gastroesophageal reflux disease (GERD), and therefore are factors in reflux esophagitis, include the following:
- Eating immediately before going to bed.
- Excessively large and fatty meals.
- Smoking.
- Extra weight, including from pregnancy.
Several foods may worsen symptoms of GERD or reflux esophagitis:
- Caffeine.
- Alcohol.
- Fatty foods.
- Chocolate.
- Peppermint.
Eosinophilic esophagitis
Risk factors for eosinophilic esophagitis, or allergy-related esophagitis, may include:
- A history of certain allergic reactions, including asthma, atopic dermatitis and allergic rhinitis, also known as hay fever.
- A family history of eosinophilic esophagitis.
Drug-induced esophagitis
Factors that may increase the risk of drug-induced esophagitis are generally related to issues that prevent quick and complete passage of a pill into the stomach. These factors include:
- Swallowing a pill with little or no water.
- Taking drugs while lying down.
- Taking drugs right before sleep, probably due in part to the production of less saliva and swallowing less during sleep.
- Older age, possibly because of age-related changes to the muscles of the esophagus or a decreased production of saliva.
- Large or oddly shaped pills.
Infectious esophagitis
Risk factors for infectious esophagitis often relate to medications, such as steroids or antibiotics. People with diabetes also are at increased risk of candida esophagitis in particular.
Other causes of infectious esophagitis may relate to poor immune system function. This may be due to an immune disorder, HIV/AIDS or certain cancers. Also, certain cancer treatments and drugs that block immune system reactions to transplanted organs (immunosuppressants) may increase the risk of infectious esophagitis.
Complications
Left untreated, esophagitis can lead to changes in the structure of the esophagus. Possible complications include:
- Scarring or narrowing of the esophagus, known as a stricture.
- Tearing of the esophageal lining due to retching or passing instruments through an inflamed esophagus during endoscopy.
- Barrett's esophagus, a condition in which the cells lining the esophagus are damaged from acid reflux, increasing your risk of esophageal cancer.
Diagnosis
Your health care provider or specialist will likely make a diagnosis based on your answers to questions, a physical exam, and one or more tests. These tests may include:
Endoscopy
During this procedure, a long, thin tube equipped with a tiny camera is guided down your throat and into the esophagus. This instrument is called an endoscope. Using the endoscope, your provider can look for any unusual appearance of the esophagus. Small tissue samples may be taken for testing. This is called a biopsy. The esophagus may look different depending on the cause of the inflammation, such as drug-induced or reflux esophagitis. You'll be lightly sedated during this test.
Esophageal sponge
This test can be performed in the health care provider's office. It involves swallowing a capsule attached to a string. The capsule will dissolve in your stomach and release a sponge that the provider will pull out of your mouth with the string. As the sponge is pulled out, it will sample the esophageal tissues. This may allow your provider to determine the degree of inflammation in your esophagus without an endoscopy.
Barium X-ray
For this test, you drink a solution or take a pill containing a compound called barium. Barium coats the lining of the esophagus and stomach and makes the organs visible. These images can help identify narrowing of the esophagus, other structural changes, a hiatal hernia, tumors or other irregularities that could be causing symptoms.
Laboratory tests
Small tissue samples removed during an endoscopic exam are sent to the lab for testing. Depending on the suspected cause of the disorder, tests may be used to:
- Diagnose a bacterial, viral or fungal infection.
- Determine the concentration of allergy-related white blood cells, called eosinophils.
- Identify irregular cells that would indicate esophageal cancer or precancerous changes.
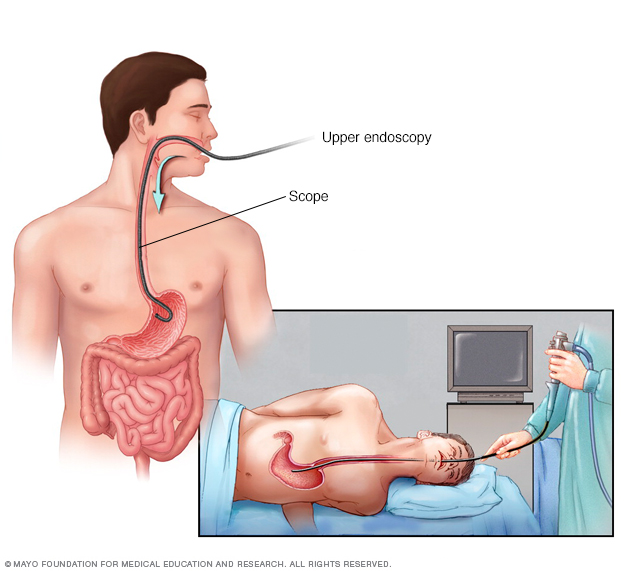
During an upper endoscopy, a healthcare professional inserts a thin, flexible tube equipped with a light and camera down the throat and into the esophagus. The tiny camera provides a view of the esophagus, stomach and the beginning of the small intestine, called the duodenum.
Treatment
Treatments for esophagitis are intended to lessen symptoms, manage complications and treat underlying causes of the disorder. Treatment strategies vary based on the cause of the disorder.
Reflux esophagitis
Treatment for reflux esophagitis may include:
- Nonprescription treatments. These include antacids (Maalox, Mylanta, others); medicines that reduce acid production, called H-2-receptor blockers, such as cimetidine (Tagamet HB); and medicines that block acid production and heal the esophagus, called proton pump inhibitors. These include lansoprazole (Prevacid) and omeprazole (Prilosec), among others.
- Prescription medicines. These include prescription-strength H-2-receptor blockers and proton pump inhibitors.
-
Surgery. A type of surgery called fundoplication may be used to improve the condition of the esophagus if other interventions don't work. In this procedure, a portion of the stomach is wrapped around the valve separating the esophagus and stomach, called the lower esophageal sphincter. This strengthens the sphincter and prevents acid from backing up into the esophagus.
A newer treatment involves placing a ring of tiny magnetic titanium beads around the lower esophageal sphincter, known as the LINX procedure. In that position, the ring of beads strengthens the sphincter, preventing acid reflux.
Eosinophilic esophagitis
Treatment for eosinophilic esophagitis involves avoiding the allergen and reducing the allergic reaction with medicines. Recommended medicines may include:
- Proton pump inhibitors. Your health care provider will likely first prescribe a proton pump inhibitor, such as esomeprazole (Nexium), lansoprazole (Prevacid), omeprazole (Prilosec) or pantoprazole (Protonix).
-
Steroids. Some studies have shown that swallowed steroids such as fluticasone (Flovent) and budesonide (Pulmicort) may act on the surface tissue of the esophagus to treat eosinophilic esophagitis. The same steroid medications that are inhaled to manage asthma are swallowed in a liquid form to treat eosinophilic esophagitis.
Your health care provider will instruct you on how to swallow the steroid preparation so that it coats your esophagus. This delivery system of steroids is much less likely to cause serious side effects than taking oral steroid pills.
-
Elimination and elemental diets. A response to a food allergen is likely the cause of eosinophilic esophagitis. Therefore, elimination of the culprit food may be an effective treatment strategy.
Because no reliable tests are currently available to identify the culprit food, your provider may recommend that you remove common food allergens from your diet. Under your provider's direction, you'll gradually add foods back into your diet and note when symptoms return.
Another, more restrictive, approach is to remove all food from your diet and replace it with an amino acid-based formula.
- Monoclonal antibodies. The Food and Drug Administration (FDA) recently approved dupilumab (Dupixent) for treatment of adults and children 12 years and older with eosinophilic esophagitis. Dupilumab is a type of medicine known as a monoclonal antibody. It works to block the action of certain proteins in the body that cause inflammation. Dupilumab is given weekly via injection.
Drug-induced esophagitis
Treatment for drug-induced esophagitis involves not using the problem drug when possible and reducing the risk with better pill-taking habits. Your provider may recommend:
- Taking an alternative medicine that is less likely to cause drug-induced esophagitis.
- Taking a liquid version of a medicine if possible.
- Drinking an entire glass of water with a pill, unless you've been told by your provider to restrict your fluid intake because of another condition, such as kidney disease.
- Sitting or standing for at least 30 minutes after taking a pill.
Infectious esophagitis
Your provider may prescribe a medicine to treat a bacterial, viral, fungal or parasitic infection causing infectious esophagitis.
Treating common complications
A gastroenterologist may perform a procedure to expand, or dilate, the esophagus. This treatment is generally used only when the narrowing is very severe or food has become stuck in the esophagus.
In esophageal dilation, your provider uses one or more endoscopic devices. These are small narrow tubes inserted through the esophagus. Versions of these devices may be equipped with:
- A tapered tip that starts with a rounded point that gradually widens.
- A balloon that can be expanded after it's inserted in the esophagus.
Lifestyle and home remedies
Depending on the type of esophagitis you have, you may lessen symptoms or stop recurring problems by following these steps:
- Do not eat foods that may increase reflux. Eating or drinking large amounts of certain foods may worsen your symptoms of gastroesophageal reflux. These may include alcohol, caffeine, chocolate and mint-flavored foods.
- Use good pill-taking habits. Always take a pill with plenty of water. Don't lie down for at least 30 minutes after taking a pill.
- Lose weight. Talk to your health care provider about an appropriate diet and exercise routine to help you lose weight and maintain a healthy weight.
- If you smoke, quit. Talk to your provider if you need help ending a smoking habit.
- Try not to stoop or bend, especially soon after eating.
- Do not lie down after eating. Wait at least three hours after eating to lie down or go to bed.
- Raise the head of your bed. Place wooden blocks under your bed to elevate your head. Aim for an elevation of 6 to 8 inches (15 to 20 centimeters). If it's not possible to elevate your bed, insert a wedge between your mattress and box spring to elevate your body from the waist up. Raising your head by using only pillows isn't effective.
Alternative medicine
No alternative medicine therapies have been proved to treat esophagitis. Still, some complementary and alternative therapies may provide some relief from heartburn or reflux symptoms when combined with your health care provider's care. Options may include ginger, chamomile and slippery elm. Talk to your health care provider if you're considering taking alternative therapies to treat GERD.
Preparing for an appointment
If you're experiencing severe chest pain that lasts more than a few minutes or if you suspect you have food lodged in your esophagus or are not able to swallow, get emergency medical care.
If you have other symptoms of esophagitis, you'll likely start by seeing your primary health care provider. For some diagnostic tests, your provider may refer you to a specialist in digestive system disorders (gastroenterologist) or an allergy specialist (allergist). Preparing for your appointment with your provider or a specialist will help you make the best use of your time.
What you can do
Make a list ahead of time, including:
- Symptoms you're experiencing, including any that may seem unrelated to pain, difficulty swallowing or reflux.
- Key personal information, including any major stresses or recent life changes.
- Medications that you're taking, including vitamins and other supplements.
- Family history of allergies and disorders of the esophagus or stomach.
- Questions to ask your health care provider.
List questions from most important to least important in case time runs out. If you think you have symptoms of esophagitis, you may ask some of the following:
- What tests will I need to diagnose the condition?
- Do these tests require any special preparation?
- How long will it take to find out the results of tests?
- What treatments are available, and which do you recommend?
- How will we know if the treatment is working?
- Will I need follow-up tests?
- What steps can I take on my own to prevent symptoms from happening again?
- I have other medical conditions. How can I best manage these conditions together?
What to expect from your doctor
Your provider is likely to ask you a number of questions. Being ready to answer them may reserve time to go over points you want to spend more time on. Your provider may ask:
- How severe is your pain or discomfort?
- Do you have difficulty swallowing?
- How often do you experience symptoms?
- Does anything seem to prompt or worsen symptoms, such as certain foods?
- Does anything lessen symptoms, such as taking nonprescription antacids or not eating certain foods?
- Are symptoms worse at certain times of the day?
- Do your symptoms begin shortly after taking any medications? If so, which medications?
- Do you have any allergies, and do you take any allergy medicine?
- Have you ever had food get stuck in your throat after swallowing?
- Do you ever have food come back up after swallowing?
- Do you have a family history of gastrointestinal problems?
What you can do in the meantime
If you know that certain foods trigger or worsen symptoms, stay away from them. Common culprits include caffeine-containing drinks, alcohol or spicy foods. Taking nonprescription antacids may provide short-term relief of symptoms.
If you suspect that your symptoms are related to a prescription medicine, don't stop taking the medicine without first talking to your health care provider. If possible, limit the use of nonprescription medications that could be causing problems. When you take pills, drink a glass of water and don't lie down immediately afterward.
Last Updated Nov 29, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



