Fibromuscular dysplasia
Overview
Fibromuscular dysplasia is a condition that causes the medium-sized arteries in the body to narrow and grow larger. Narrowed arteries can reduce blood flow and affect how body organs work.
Fibromuscular dysplasia is most often seen in the arteries leading to the kidneys and brain. But it also can affect arteries in the legs, heart, belly area and, rarely, the arms. More than one artery can be involved.
Treatments are available to control symptoms and help prevent complications, such as stroke. But there is no cure for fibromuscular dysplasia.
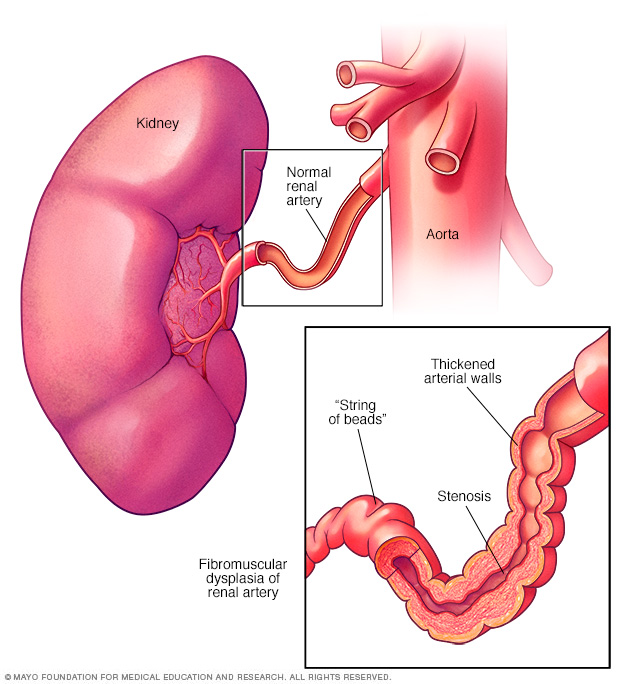
In fibromuscular dysplasia, the muscle and fiber tissues in the arteries thicken, causing the arteries to narrow. This is called stenosis. Narrowed arteries can reduce blood flow to the organs, causing organ damage. The artery to the kidney is called the renal artery. Fibromuscular dysplasia of the renal artery is shown here, with a "string of beads" appearance.
Symptoms
Symptoms of fibromuscular dysplasia depend on which artery or arteries are affected. Some people don't have any symptoms.
If the arteries to the kidneys are affected, common symptoms include:
- High blood pressure.
- Problems with how the kidneys work.
If the arteries affected supply blood to the brain, symptoms might include:
- Headache.
- A pulsing feeling or ringing sound in your ears, called tinnitus.
- Dizziness.
- Sudden neck pain.
- Stroke or transient ischemic attack.
When to see a doctor
If you have fibromuscular dysplasia, get medical help immediately if you have symptoms of a stroke, such as:
- Sudden changes in vision.
- Sudden changes in the ability to speak.
- Sudden or new weakness in the arms or legs.
If you are concerned about your risk of fibromuscular dysplasia, make an appointment for a health checkup. The condition can rarely run in families. But there's no genetic test for fibromuscular dysplasia.
Causes
The cause of fibromuscular dysplasia is not known. Changes in genes might cause the condition.
Because the condition is more common in women than men, researchers think female hormones also may play a role. But exactly how is unclear. Fibromuscular dysplasia is not linked to women's use of birth control pills.
Risk factors
Things that increase the risk of fibromuscular dysplasia include:
- Sex. The condition is more common in women than it is in men.
- Age. Fibromuscular dysplasia tends to be diagnosed in people in their 50s. But it can affect anyone of any age.
- Smoking. People who smoke seem to have an increased risk of developing fibromuscular dysplasia. Smoking also can make the disease worse.
Complications
Possible complications of fibromuscular dysplasia include:
- High blood pressure. The narrowing of the arteries of the kidneys causes higher pressure on the artery walls. Damage to the arteries may lead to heart disease or heart failure.
- Tears in the artery walls. Fibromuscular dysplasia and tears in the walls of the arteries often occur together. An artery tear is called a dissection. When a tear forms in one of the blood vessels in the heart, it's called a spontaneous coronary artery dissection (SCAD). A dissection can slow or block blood flow. Emergency medical treatment is needed.
- Bulge or ballooning of an artery. Also called an aneurysm, this complication can occur if the artery wall is weak or damaged. Fibromuscular dysplasia can weaken the walls of the affected arteries. An aneurysm that breaks open, called a rupture, can be life-threatening. Emergency medical treatment is needed for a ruptured aneurysm.
- Stroke. An artery tear or aneurysm rupture in the brain can lead to stroke. High blood pressure also can increase the risk of a stroke.
Diagnosis
A member of your health care team examines you and asks questions about your family and medical history. A device called a stethoscope is used to listen to blood flow through the arteries in the neck and belly area. If you have fibromuscular dysplasia, the provider might hear an irregular sound due to narrowed arteries.
If someone in your family has or had fibromuscular dysplasia, you may need tests to check for it even if you don't have symptoms.
Tests
Tests to diagnose fibromuscular dysplasia could include:
- Blood tests. Blood tests may be done to check for signs of other conditions that can narrow arteries. You may have your blood sugar and cholesterol levels checked.
- Duplex ultrasound. This imaging test can show if an artery is narrowed. It uses sound waves to create pictures of blood flow and the shape of blood vessels. During the test, a wand-like device is pressed to the skin over the affected area.
- Angiogram. This is a commonly used test for fibromuscular dysplasia. A doctor inserts a thin tube called a catheter into an artery. The tube is moved until it reaches the area being examined. Dye is given into a vein. Then, X-rays are used to create pictures of the arteries. The dye helps the arteries show up more clearly on the X-ray images.
- CT angiogram. This test is done using a computerized tomography (CT) machine. It provides cross-sectional images of the body. It can show narrowing in the arteries, aneurysms and dissections. You lie on a narrow table, which slides through a doughnut-shaped scanner. Before the test starts, dye called contrast is given into a vein. The dye helps blood vessels show up more clearly on the images.
- Magnetic resonance (MR) angiogram. This test uses a magnetic field and radio waves to create images of the body. It can see if you have an aneurysm or artery tear. During the test, you lie on a narrow table that slides into a tubelike machine that's open on both ends. Before the test starts, you might be given dye into a vein. The dye, called contrast, helps blood vessels show up more clearly on the test images.
The most common form of fibromuscular dysplasia looks like a "string of beads" on imaging tests. Other forms of fibromuscular dysplasia may look smooth.
Treatment
Treatment for fibromuscular dysplasia depends on:
- The area of the narrowed artery.
- Your symptoms.
- Any other health conditions you have, such as high blood pressure.
Some people only need regular health checkups. Other treatments may include medicines and procedures to open or repair an artery. If your symptoms change or if you have an aneurysm, you may need repeated imaging tests to check your arteries.
Medications
If you have fibromuscular dysplasia and high blood pressure, medicines are usually given to control blood pressure.
Types of medicines that may be used include:
- Angiotensin-converting enzyme (ACE) inhibitors, such as benazepril (Lotensin), enalapril (Vasotec) or lisinopril (Zestril), help relax blood vessels.
- Angiotensin 2 receptor blockers. These medicines also help relax blood vessels. Examples include candesartan (Atacand), irbesartan (Avapro), losartan (Cozaar) and valsartan (Diovan).
- Diuretics. Sometimes called water pills, these medicines help remove excess fluid from the body. A diuretic is sometimes used with other blood pressure medicines. Hydrochlorothiazide (Microzide) is an example of this type of medicine.
- Calcium channel blockers, such as amlodipine (Norvasc), nifedipine (Procardia XL) and others, help relax blood vessels.
- Beta blockers, such as metoprolol (Lopressor, Toprol XL), atenolol (Tenormin) and others, slow the heartbeat.
Some medicines used to treat high blood pressure can affect the way the kidneys work. You may need regular blood and urine tests to make sure your kidneys are working as they should.
Your doctor also might tell you take a daily aspirin to reduce your risk of stroke. But don't start taking an aspirin without talking to your health care team first.
Surgery or other procedures
Treatments may be needed to repair a narrowed or damaged artery. These may include:
- Percutaneous transluminal angioplasty (PTA). This treatment uses a thin flexible tube called a catheter and a tiny balloon to widen a narrowed artery. It helps improve blood flow to the affected area. A metal mesh tube called a stent may be placed inside the weakened part of the artery to keep it open.
- Surgery to repair or replace the damaged artery. Also called surgical revascularization, this treatment is rarely recommended. But it may be suggested if you have severe narrowing of the arteries and angioplasty isn't an option. The type of surgery done depends on the location of the narrowed artery and the amount of damage.
Preparing for an appointment
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance. For example, you might be told not to eat or drink for several hours before some tests.
Make a list of:
- Your symptoms and when they began.
- Important personal information, including any family history of fibromuscular dysplasia, aneurysms, heart disease, stroke or high blood pressure.
- All medications, vitamins or other supplements you take, including doses.
- Questions to ask your doctor.
For fibromuscular dysplasia, some basic questions to ask your doctor include:
- What's the most likely cause of my symptoms?
- What tests will I need?
- What treatments are available? What do you recommend for me?
- What's an appropriate level of physical activity?
- How often should I have health checkups if I have fibromuscular dysplasia?
- I have other health conditions. How can I best manage these conditions together?
- Should I see a specialist?
- Are there brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- Do you always have symptoms, or do they come and go?
- How severe are your symptoms?
- Does anything seem to improve your symptoms?
- What, if anything, appears to make your symptoms worse?
Last Updated Jul 28, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use