Retinal diseases
Overview
Retinal diseases vary widely, but most of them cause visual symptoms. Retinal diseases can affect any part of your retina, a thin layer of tissue on the inside back wall of the eye.
The retina contains millions of light-sensitive cells, called rods and cones, and other nerve cells that receive and organize visual information. The retina sends this information to the brain through the optic nerve, enabling you to see.
Treatment is available for some retinal diseases. Depending on your condition, treatment goals may be to stop or slow the disease. This may help preserve, improve or restore your vision. Untreated, some retinal diseases can cause severe vision loss or blindness.
Types
Common retinal diseases and conditions include:
- Retinal tear. A retinal tear occurs when the clear, gel-like substance in the center of your eye, called vitreous, shrinks and tugs on the thin layer of tissue lining the back of your eye, called the retina. This can cause a tear in the retinal tissue. It's often accompanied by the sudden onset of symptoms such as floaters and flashing lights.
- Retinal detachment. A retinal detachment is defined by the presence of fluid under the retina. This usually occurs when fluid passes through a retinal tear, causing the retina to lift away from the underlying tissue layers.
- Diabetic retinopathy. If you have diabetes, the tiny blood vessels in the back of your eye can deteriorate and leak fluid into and under the retina. This causes the retina to swell, which may blur or distort your vision. Or you may develop new, irregular capillaries that break and bleed. This also worsens your vision.
- Epiretinal membrane. Epiretinal membrane is a delicate tissue-like scar or membrane that looks like crinkled cellophane lying on top of the retina. This membrane pulls up on the retina, which distorts your vision. Objects may appear blurred or crooked.
- Macular hole. A macular hole is a small defect in the center of the retina at the back of the eye, called the macula. The hole may develop from atypical traction between the retina and the vitreous, or it may follow an injury to the eye.
- Macular degeneration. In macular degeneration, the center of the retina begins to deteriorate. This causes symptoms such as blurred central vision or a blind spot in the center of the visual field. There are two types — wet macular degeneration and dry macular degeneration. Many people will first have the dry form, which can progress to the wet form in one or both eyes.
- Retinitis pigmentosa. Retinitis pigmentosa is an inherited degenerative disease. It slowly affects the retina and causes loss of night and side vision.
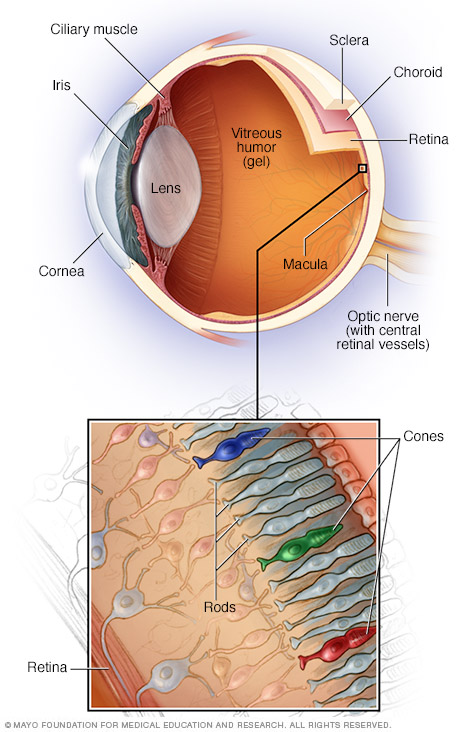
Your eye is a complex and compact structure measuring about 1 inch (2.5 centimeters) in diameter. It receives millions of pieces of information about the outside world, which are quickly processed by your brain.
Symptoms
Many retinal diseases share some common symptoms. These may include:
- Seeing floating specks or cobwebs.
- Blurred or distorted vision in which straight lines can look wavy.
- Defects in the side vision.
- Vision loss.
You may need to try looking with each eye alone to notice these changes.
When to see a doctor
It's important to pay attention to any changes in your vision and find care quickly. Seek immediate medical attention if you suddenly have floaters, flashes or reduced vision. These are warning signs of potentially serious retinal disease.
Risk factors
Risk factors for retinal diseases might include:
- Aging.
- Smoking.
- Being obese.
- Having diabetes or other diseases.
- Eye trauma.
- A family history of retinal diseases.
Treatment
The main goals of treatment are to stop or slow disease progression and preserve, improve or restore your vision. In many cases, damage that has already happened can't be reversed, making early detection important. Your eye doctor will work with you to decide on the best treatment.
Treatment of retinal disease may be complex and sometimes urgent. Options include:
- Using a laser. Laser surgery can repair a retinal tear or hole. Your surgeon uses a laser to heat small pinpoints on the retina. This creates scarring that usually binds the retina to the underlying tissue. Immediate laser treatment of a new retinal tear can decrease the chance of it causing a retinal detachment.
- Shrinking irregular blood vessels. Your eye doctor may use a technique called scatter laser photocoagulation to shrink irregular new blood vessels that are bleeding or threatening to bleed into the eye. This treatment may help people with diabetic retinopathy. Extensive use of this treatment may cause the loss of some side (peripheral) or night vision.
- Freezing. In this process, called cryopexy (KRY-o-pek-see), your surgeon applies a freezing probe to the outside wall of the eye to treat a retinal tear. Intense cold reaches the inside of the eye and freezes the retina. The treated area will later scar and secure the retina to the eye wall.
- Injecting air or gas into your eye. This technique, called pneumatic retinopexy (RET-ih-no-pek-see), is used to help repair certain types of retinal detachment. It can be used in combination with cryopexy or laser photocoagulation.
- Indenting the surface of your eye. This surgery, called scleral (SKLAIR-ul) buckling, is used to repair a retinal detachment. Your surgeon sews a small piece of silicone material to the outside eye surface, called the sclera. This indents the sclera and relieves some of the force caused by the vitreous tugging on the retina and reattaches the retina. This technique may be used with other treatments.
-
Evacuating and replacing the fluid in the eye. In this procedure, called vitrectomy (vih-TREK-tuh-me), your surgeon removes the gel-like fluid that fills the inside of your eye, called the vitreous. Air, gas or liquid is then injected into the space.
Vitrectomy may be used if bleeding or inflammation clouds the vitreous and blocks the surgeon's view of the retina. This technique may be part of the treatment for people with a retinal tear, diabetic retinopathy, a macular hole, epiretinal membrane, an infection, eye trauma or a retinal detachment.
- Injecting medicine into the eye. Your eye doctor may suggest injecting medicine into the vitreous in the eye. This technique may be effective in treating people with wet macular degeneration, diabetic retinopathy or broken blood vessels within the eye.
- Implanting a retinal prosthesis. People who have severe vision loss or blindness owing to certain inherited retinal disease may need surgery. A tiny electrode chip is implanted in the retina that receives input from a video camera on a pair of eyeglasses. The electrode picks up and relays visual information that the damaged retina can no longer process.
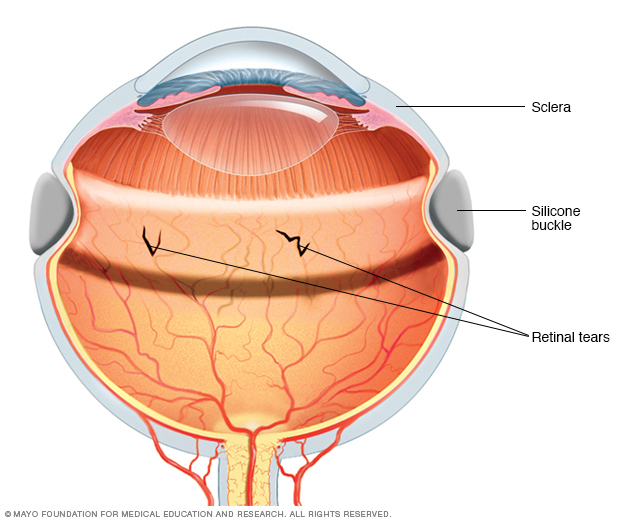
Silicone material stitched to the outside of the eye indents (buckles) the sclera, causing a slight decrease in the circumference of the eye. A scleral buckle is sometimes used in the management of retinal detachment.
Coping and support
Vision loss from retinal disease can affect your ability to do things such as read, recognize faces and drive. These tips may help you cope with your changing vision:
- Ask your eye doctor to check your eyeglasses. If you wear contacts or glasses, be sure your prescription is up to date and at maximum strength. If a stronger pair of glasses doesn't help, ask for a referral to a low-vision specialist.
- Use prescribed magnifiers. A variety of magnifying devices prescribed by a low-vision specialist can help you with reading and close-up work, such as sewing. Such devices include hand-held lenses or magnifying lenses you wear like glasses. You also may use a closed-circuit television system that uses a video camera to magnify reading material and project it on a video screen. Over-the-counter magnifiers may not work as well.
- Change your computer display and add audio systems. Adjust the font size and monitor contrast in your computer's settings. Consider adding speech-output systems or other technologies to your computer.
- Use electronic reading aids and voice interface. Try talking watches, clocks and calculators; large-print books; tablet computers; and audio books. Some tablet and smartphone apps are designed to help people with low vision. And many of these devices now come with a voice recognition feature.
- Select special appliances made for low vision. Some clocks, radios, telephones and other appliances have extra-large numbers. You may find it easier to watch a television with a larger high-definition screen, or you may want to sit closer to the screen.
- Use brighter lights in your home. Better lighting helps with reading and other daily activities, and it also may reduce the risk of falling.
- Consider your transportation options. If you drive, check with your doctor to see if it's safe to continue doing so. Be extra cautious in certain situations, such as driving at night, in heavy traffic or in bad weather. Use public transportation or ask a friend or family member to help. Make arrangements to use local van or shuttle services, volunteer driving networks, or ride-shares.
- Get support. Having a retinal condition can be difficult, and you may need to make changes in your life. You may go through many emotions as you adjust. Consider talking to a counselor or joining a support group. Spend time with supportive family members and friends.
Preparing for an appointment
To check for retinal disease, a dilated eye exam is usually necessary. Make an appointment with a doctor who specializes in eye care — an optometrist or an ophthalmologist. He or she can perform a complete eye exam.
What you can do
Before your appointment:
- When you make the appointment, ask if you need to do anything to prepare.
- List any symptoms you're experiencing, including those that seem unrelated to your vision problem.
- List all medications, vitamins and supplements you take, including doses.
- Ask a family member or friend to accompany you. Having your pupils dilated for the eye exam will affect your vision for a time afterward, so you may need someone to drive or accompany you after your appointment.
- List questions to ask your doctor.
For retinal disease, questions to ask your doctor include:
- How advanced is my condition?
- Is it safe for me to drive?
- Will I experience further vision loss?
- Can my condition be treated?
- Will taking a vitamin or mineral supplement help prevent further vision loss?
- What's the best way to monitor my vision for any changes?
- What changes in my symptoms warrant calling you?
- What low-vision aids might be helpful to me?
- What lifestyle changes can I make to protect my vision?
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did you first notice your vision problem?
- Does the condition affect one or both eyes?
- Do you have trouble seeing things near you, at a distance or both?
- Do you smoke or did you ever smoke? If so, how much?
- Do you have other medical problems, such as high cholesterol, high blood pressure or diabetes?
- Do you have a family history of retinal disease?
- Have you experienced an injury to your eye?
Last Updated Mar 8, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use