HPV test
Overview
Human papillomavirus, also called HPV, that is spread through sexual activity can cause genital warts, changes in cervical cells or cancers. The HPV test looks for evidence of the virus in samples from the body. This test may be done at the same time or after another screening test called a Pap test or Pap smear.
Your healthcare professional might suggest the HPV test if:
- Your Pap test results are not clear. This is called atypical squamous cells of undetermined significance, shortened to ASCUS.
- You're age 30 or older.
- You've had atypical cervical cancer screening results in the past.
The HPV test is approved only for cells from the cervix. If you had surgery to remove the uterus, called hysterectomy, because of cervical cancer or abnormal cervical cells, the HPV test may be used to test cells of the vagina. A healthcare professional may suggest an HPV test for cells from the anus. HPV testing on anal cells is not suggested in general. But some groups of people who are at higher risk than average may benefit from the screening.
People with HIV
Screening of anal cells for HPV may be suggested starting at age 35 for transgender women who have HIV, and men who have sex with men who have HIV. For others who have HIV, screening may start at age 45.
People who've had a transplant
Solid organ transplant recipients starting 10 years after transplant may benefit from HPV screening using anal cells. Screening may be recommended earlier for females who are 5 to 9 years out from a solid organ transplant.
People with pre-cancer or cancer of vulvar cells
People with severely atypical vulvar cells or vulvar cancer who may start anal cell HPV screening within a year of diagnosis.
Why it's done
The HPV test screens for cancer of the lower, narrow end of the uterus that's at the top of the vagina, called the cervix. But the test doesn't show cancer. Instead, the test shows HPV, the virus that causes cervical cancer. Certain types of HPV increase cervical cancer risk.
Knowing that you have a type of HPV that puts you at high risk of cervical cancer helps you and your healthcare team decide on the next steps in your care. Those steps might include your having repeat HPV and Pap tests. Or your healthcare professional may recommend taking a sample of the cervix for testing, called a biopsy. You may also need treatment for precancerous cells.
A positive HPV test doesn't mean that you'll get cervical cancer. But it does mean that your healthcare professional may suggest screening more often or for longer than is typical.
Many guidelines don't suggest testing under age 30 for HPV. But talk with your healthcare professional about about the right time for you to test for HPV.
The infections most often become inactive, called dormant, or go away on their own with no lasting cell changes to the cervix. Dormant infections may stay inactive for years and then become active again.
Cervical changes that lead to cancer can take years to show up. So if you test positive for HPV, you might have watchful waiting instead of treatment for cervical changes caused by an HPV infection.
Risks
As with any screening test, an HPV test carries the risk of false-positive or false-negative results.
- False-positive. A false-positive test result shows that you have a high-risk type of HPV when you don't. A false-positive result could lead to follow-up tests that you don't need. These can include a repeat test or cervical biopsy. False-positives are rare, but they can cause worry.
-
False-negative. A false-negative test result means that you do have an HPV infection, but the test shows that you don't. This might cause a delay in getting follow-up tests.
You can have HPV, but the test can be negative. This may mean that your body is controlling the HPV infection. But the HPV is still in your body. A future test can be positive without new contact with HPV.
How you prepare
You don't need to do anything before you have an HPV test. But since an HPV test often is done at the same time as a Pap test, you can take these measures to help both tests be correct:
- Don't have intercourse for two days before the test. Also don't douche or use vaginal medicines or sperm-killing foams, creams or jellies.
- Try not to have the test during your menstrual period. The test can be done, but your healthcare professional can collect a better sample of cells at another time in your cycle.
What you can expect
An HPV test most often is done at the same time as a Pap test. A Pap test looks for cancer in cells from your cervix. An HPV test can be done using the sample from the Pap test. Or your healthcare professional can get a second sample from the cervical canal.
During the procedure
A combined Pap-HPV test is done in your healthcare professional's office. It takes only a few minutes. You may be asked to take off all your clothes or to take off clothes only from the waist down.
You lie on your back on an exam table with your knees bent. Your heels rest in supports called stirrups.
Your healthcare professional gently puts a device called a speculum into your vagina. The speculum holds the walls of the vagina apart so that your care professional can see your cervix. When the speculum goes in, you may feel pressure in your pelvic area. And the speculum can feel cold at first.
Then your care professional takes samples of your cervical cells using a soft brush and a flat scraping device called a spatula. You may feel mild cramping for a short time. Or you may not feel the sample being taken.
After the procedure
After your test, you can go about your daily activities as usual. Ask when you will get your test results.
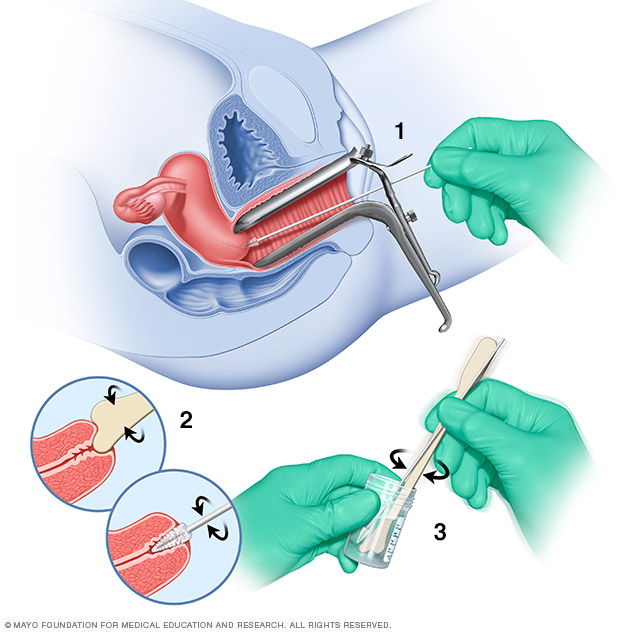
During a Pap test, a tool called a speculum holds the vaginal walls apart. A sample of cells from the cervix is collected using a soft brush and a flat scraping device called a spatula (1 and 2). The cells are placed in a bottle that contains a solution to preserve them (3). Or the cells may be smeared onto a glass slide. Later, the cells are checked under a microscope.
Results
Results from your HPV test come back as positive or negative.
Positive HPV test
A positive test result means that you have a type of high-risk HPV that's linked to cervical cancer. It doesn't mean that you have or will get cervical cancer. But it's a warning that you could get cervical cancer.
Depending on other results, your healthcare professional may suggest a procedure to take a closer look at your cervix. This is called a colposcopy. Or your healthcare professional may suggest a follow-up HPV test in a year to see if the infection is gone or to check for signs of cervical cancer.
Negative HPV test
A negative test result means that you don't have any of the types of HPV that cause cervical cancer or that your body has the HPV infection under control.
Depending on your test results, your healthcare professional may suggest one of the following as a next step:
- Watching. If you're over age 30, you can repeat the Pap and HPV tests in five years if your HPV test is negative, your Pap test is OK and you haven't had positive tests before. If you've had positive results before, you may need follow-up testing in one or three years.
- Colposcopy. In this follow-up procedure, your healthcare professional uses a special lens called a colposcope to look closely at your cervix.
- Biopsy. In this procedure, often done with colposcopy, your healthcare professional takes a sample of cervical cells to be looked at under a microscope.
- Taking out cervical cells that are severely abnormal. To keep these cells from turning into cancer, you might have a procedure to remove the tissue that has those cells. Milder changes can pose a low risk of cancer and may heal without treatment.
- Seeing a specialist. If your Pap test or HPV test results are positive, your healthcare professional will likely refer you to a healthcare professional trained in colposcopy. If test results show that you might have cancer, you may be sent to a specialist in treating cancers of the female genital tract, called a gynecologic oncologist, for treatment.
Last Updated Jul 13, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use