Craniosynostosis
Overview
Craniosynostosis (kray-nee-o-sin-os-TOE-sis) is a disorder present at birth in which one or more of the fibrous joints between the bones of your baby's skull (cranial sutures) close prematurely (fuse), before your baby's brain is fully formed. Brain growth continues, giving the head a misshapen appearance.
Usually, during infancy the sutures remain flexible, allowing a baby's skull to expand as the brain grows. In the front of the skull, the sutures meet in the large soft spot (fontanel) on top of the head. The anterior fontanel is the soft spot felt just behind a baby's forehead. The next largest fontanel is at the back (posterior). Each side of the skull has a tiny fontanel.
Craniosynostosis usually involves premature fusion of a single cranial suture, but it can involve more than one of the sutures in a baby's skull (multiple suture craniosynostosis). In rare cases, craniosynostosis is caused by certain genetic syndromes (syndromic craniosynostosis).
Treating craniosynostosis involves surgery to correct the shape of the head and allow for brain growth. Early diagnosis and treatment allow your baby's brain adequate space to grow and develop.
Although neurological damage can occur in severe cases, most children develop as expected in their ability to think and reason (cognitive development) and have good cosmetic results after surgery. Early diagnosis and treatment are key.
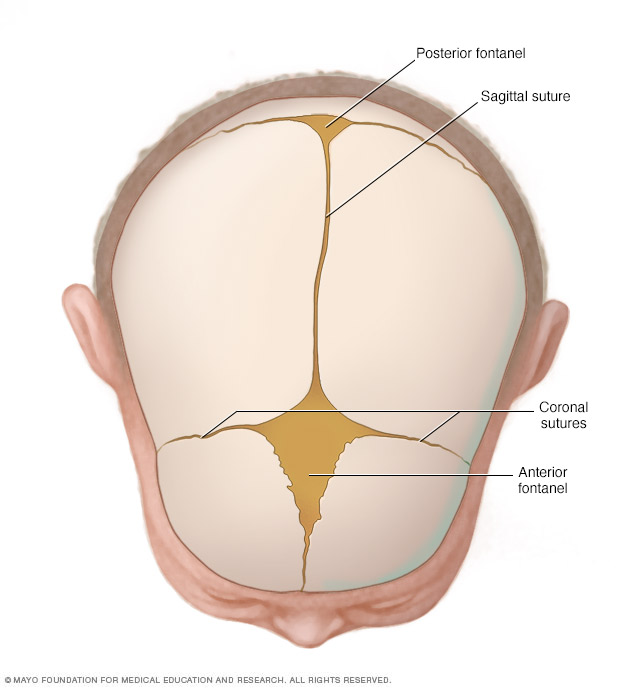
Joints made of strong, fibrous tissue (cranial sutures) hold the bones of your baby's skull together. The sutures meet at the fontanels, the soft spots on your baby's head. The sutures remain flexible during infancy, allowing the skull to expand as the brain grows. The largest fontanel is at the front (anterior).
Symptoms
The signs of craniosynostosis are usually noticeable at birth, but they become more apparent during the first few months of your baby's life. Signs and severity depend on how many sutures are fused and when in brain development the fusion occurs. Signs and symptoms can include:
- A misshapen skull, with the shape depending on which of the sutures are affected
- Development of a raised, hard ridge along affected sutures, with a change in the shape of the head that's not typical
Types of craniosynostosis
There are several types of craniosynostosis. Most involve the fusion of a single cranial suture. Some complex forms of craniosynostosis involve the fusion of multiple sutures. Multiple suture craniosynostosis is usually linked to genetic syndromes and is called syndromic craniosynostosis.
The term given to each type of craniosynostosis depends on what sutures are affected. Types of craniosynostosis include:
- Sagittal (scaphocephaly). Premature fusion of the sagittal suture that runs from the front to the back at the top of the skull forces the head to grow long and narrow. This head shape is called scaphocephaly. Sagittal craniosynostosis is the most common type of craniosynostosis.
- Coronal. Premature fusion of one of the coronal sutures (unicoronal) that run from each ear to the top of the skull may cause the forehead to flatten on the affected side and bulge on the unaffected side. It also leads to turning of the nose and a raised eye socket on the affected side. When both coronal sutures fuse prematurely (bicoronal), the head has a short and wide appearance, often with the forehead tilted forward.
- Metopic. The metopic suture runs from the top of the bridge of the nose up through the midline of the forehead to the anterior fontanel and the sagittal suture. Premature fusion gives the forehead a triangular appearance and widens the back part of the head. This head shape is also called trigonocephaly.
- Lambdoid. Lambdoid synostosis is a rare type of craniosynostosis that involves the lambdoid suture, which runs along the back of the head. It may cause one side of a baby's head to appear flat, one ear to be higher than the other ear and tilting of the top of the head to one side.
Other reasons for a misshapen head
A misshapen head doesn't always indicate craniosynostosis. For example, if the back of your baby's head appears flattened, it could be the result of spending too much time lying on one side of the head. This can be treated with regular position changes, or if significant, with helmet therapy (cranial orthosis) to help reshape the head to a more balanced appearance.
When to see a doctor
Your health care provider will routinely monitor your child's head growth at well-child visits. Talk to your pediatrician if you have concerns about your baby's head growth or shape.
Causes
Often the cause of craniosynostosis is not known, but sometimes it's related to genetic disorders.
- Nonsyndromic craniosynostosis is the most common type of craniosynostosis. Its cause is unknown, although it's thought to be a combination of genes and environmental factors.
- Syndromic craniosynostosis is caused by certain genetic syndromes, such as Apert syndrome, Pfeiffer syndrome or Crouzon syndrome, which can affect a baby's skull development. These syndromes usually also include other physical features and health problems.
Complications
If untreated, craniosynostosis may cause, for example:
- Permanently misshapen head and face
- Poor self-esteem and social isolation
The risk of increased pressure inside the skull (intracranial pressure) from simple craniosynostosis is small if the suture and head shape are fixed surgically. But babies with an underlying syndrome may develop increased intracranial pressure if their skulls don't expand enough to make room for their growing brains.
If untreated, increased intracranial pressure can cause:
- Developmental delays
- Cognitive impairment
- Blindness
- Seizures
- Headaches
Diagnosis
Craniosynostosis requires evaluation by specialists, such as a pediatric neurosurgeon or a specialist in plastic and reconstructive surgery. Diagnosis of craniosynostosis may include:
- Physical exam. Your health care provider feels your baby's head for features such as suture ridges and looks for facial differences such as unbalanced features.
- Imaging studies. A computerized tomography (CT) scan or magnetic resonance imaging (MRI) of your baby's skull can show whether any sutures have fused. Cranial ultrasound imaging may be used. Fused sutures can be identified by their absence — because they're invisible once fused — or by a ridging of the suture line. A laser scan and photographs also may be used to make precise measurements of the skull shape.
- Genetic testing. If your health care provider suspects an underlying genetic syndrome, genetic testing may help identify the syndrome.
Treatment
Mild cases of craniosynostosis may not need treatment. Your health care provider may recommend a specially molded helmet to help reshape your baby's head if the cranial sutures are open and the head is misshapen. In this situation, the molded helmet can assist your baby's brain growth and correct the shape of the skull.
However, for most babies, surgery is the primary treatment. The type and timing of surgery depends on the type of craniosynostosis and whether there's an underlying genetic syndrome. Sometimes more than one surgery is required.
The purpose of surgery is to correct the head shape, reduce or prevent pressure on the brain, create room for the brain to grow properly, and improve your baby's appearance. This involves a process of planning and surgery.
Surgical planning
Imaging studies can help surgeons develop a surgical procedure plan. Virtual surgical planning for treatment of craniosynostosis uses high-definition 3D CT scans and MRI scans of your baby's skull to construct a computer-simulated, individualized surgical plan. Based on that virtual surgical plan, customized templates are constructed to guide the procedure.
Surgery
A team that includes a specialist in surgery of the head and face (craniofacial surgeon) and a specialist in brain surgery (neurosurgeon) generally performs the procedure. Surgery can be done by endoscopic or open surgery. Both types of procedures generally produce very good cosmetic results with low risk of complications.
- Endoscopic surgery. This minimally invasive surgery may be considered for babies up to age 6 months. Surgery done early is preferred. Using a lighted tube and camera (endoscope) inserted through small scalp cuts (incisions), the surgeon removes the affected suture to allow the baby's brain to grow properly. Compared with an open procedure, endoscopic surgery has a smaller incision, typically involves only a one-night hospital stay and usually does not require a blood transfusion.
- Open surgery. Generally, open surgery is done for babies older than 6 months. The surgeon makes an incision in the scalp and cranial bones, then reshapes the affected portion of the skull. The skull position is held in place with plates and screws that are absorbable. Open surgery typically involves a hospital stay of three or four days, and a blood transfusion is usually necessary. It's generally a one-time procedure, but in complex cases, multiple open surgeries are often required to correct the baby's head shape.
Helmet therapy
After minimally invasive surgery, office visits at certain intervals are needed to fit a series of helmets to help shape your baby's skull. The surgeon will determine the length of helmet therapy based on how quickly the shape responds to treatment. If open surgery is done, usually no helmet is needed afterward.
Coping and support
When you learn that your baby has craniosynostosis, you may experience a range of emotions. You may not know what to expect. Information and support can help.
Consider these steps to prepare yourself and to care for your baby:
- Find a team of trusted professionals. You'll need to make important decisions about your baby's care. Medical centers with craniofacial specialty teams can offer you information about the disorder, coordinate your baby's care among specialists, help you evaluate options and provide treatment.
- Seek out other families. Talking to people who are dealing with similar challenges can provide you with information and emotional support. Ask your health care provider about support groups in your community. If a group isn't for you, maybe your provider can put you in touch with a family who has dealt with craniosynostosis. Or you may be able to find group or individual support online.
- Expect a bright future. Most children have appropriate cognitive development and good cosmetic results after surgery. Early diagnosis and treatment are key. When needed, early intervention services offer help with developmental delays or intellectual disabilities.
Preparing for an appointment
In some cases, your baby's pediatrician may suspect craniosynostosis at a routine well-baby visit. In other cases, you may make an appointment because you have concerns about your baby's head growth. Your health care provider can refer you to a specialist for diagnosis and treatment.
Here's some information to help you get ready for your appointment. If possible, bring a family member or friend with you. A trusted companion can help you remember information and provide emotional support.
What you can do
Before the appointment, make a list of:
- Any signs you've noticed, such as raised ridges or a change in the shape of your baby's face or head
- Questions to ask your health care provider
Questions to ask might include:
- What's the most likely cause of my baby's symptoms?
- Are there other possible causes?
- What kinds of tests does my baby need? Do these tests require any special preparation?
- What treatments are available, and which do you recommend?
- Are there alternatives to the treatment you're recommending?
- What are the risks involved with surgery?
- Who will perform the surgery if it's needed?
- What happens if we choose not to have the surgery right now?
- Will the shape of the skull affect the functioning of my baby's brain?
- What is the likelihood of future children having the same condition?
- Are there brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask other questions during the appointment.
What to expect from your doctor
Your health care provider is likely to ask you questions, such as:
- When did you first notice the changes in your baby's head?
- How much time does your baby spend on his or her back?
- In what position does your baby sleep?
- Has your baby had any seizures?
- Is your baby's development on schedule?
- Were there any complications during your pregnancy?
- Do you have a family history of craniosynostosis or genetic conditions such as Apert syndrome, Pfeiffer syndrome or Crouzon syndrome?
Your health care provider will ask additional questions based on your responses. Preparing and anticipating questions will help you make the most of your appointment.
Last Updated Sep 15, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use




