Diarrhea
Overview
Diarrhea — loose, watery and possibly more-frequent bowel movements — is a common problem. Sometimes, it's the only symptom. At other times, it may be associated with other symptoms, such as nausea, vomiting, abdominal pain or weight loss.
Luckily, diarrhea is usually short-lived, lasting no more than a few days. But when diarrhea lasts beyond a few days into weeks, it usually means that there's another problem — such as irritable bowel syndrome (IBS) or a more serious disorder, including ongoing infection, celiac disease or inflammatory bowel disease (IBD).
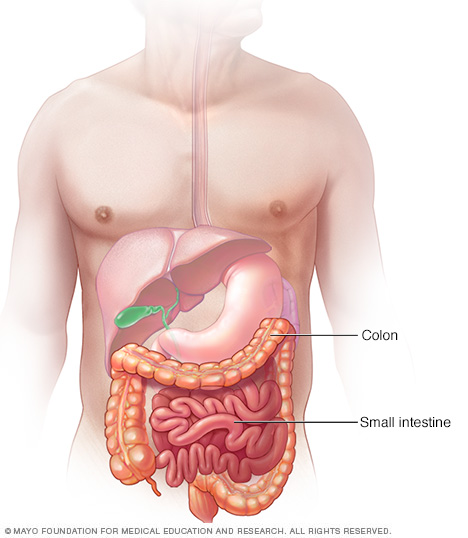
The small intestine and colon are components of your digestive tract, which processes the foods you eat. The intestines extract nutrients from the foods. What isn't absorbed by the intestines continues along the digestive tract and is expelled as stool during a bowel movement. Diarrhea can be present due to irregularities in the small intestine or the large intestine.
Symptoms
Symptoms associated with diarrhea (loose, watery stools) may include:
- Belly cramps or pain.
- Bloating.
- Nausea.
- Vomiting.
- Fever.
- Blood in the stool.
- Mucus in the stool.
- Urgent need to have a bowel movement.
When to see a doctor
If you're an adult, see your doctor if:
- Your diarrhea persists beyond two days with no improvement.
- You become dehydrated.
- You have severe abdominal or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
In children, particularly young children, diarrhea can quickly lead to dehydration. Call your doctor if your child's diarrhea doesn't improve within 24 hours or if your child:
- Becomes dehydrated.
- Has a fever above 102 F (39 C).
- Has bloody or black stools.
Causes
A number of diseases and conditions can cause diarrhea, including:
- Viruses. Viruses that can cause diarrhea include Norwalk virus (also known as norovirus), enteric adenoviruses, astrovirus, cytomegalovirus and viral hepatitis. Rotavirus is a common cause of acute childhood diarrhea. The virus that causes coronavirus disease 2019 (COVID-19) also has been associated with gastrointestinal symptoms, including nausea, vomiting and diarrhea.
- Bacteria and parasites. Exposure to certain bacteria, such as E. coli or parasites through contaminated food or water, leads to diarrhea. When traveling in developing countries, diarrhea caused by bacteria and parasites is often called traveler's diarrhea. Clostridioides difficile (also known as C. diff) is another type of bacterium that causes diarrhea, and it can occur after a course of antibiotics or during a hospitalization.
- Medicines. Many medicines, such as antibiotics, can cause diarrhea. Antibiotics get rid of infections by killing bad bacteria, but they also kill good bacteria. This disturbs the natural balance of bacteria in your intestines, leading to diarrhea or an infection such as C. diff. Other drugs that cause diarrhea are anti-cancer drugs and antacids with magnesium.
- Lactose intolerance. Lactose is a sugar found in milk and other dairy products. People who have trouble digesting lactose have diarrhea after eating dairy products. Lactose intolerance can increase with age because levels of the enzyme that helps digest lactose drop as you get older.
- Fructose. Fructose is a sugar found naturally in fruits and honey. It's sometimes added as a sweetener to certain beverages. Fructose can lead to diarrhea in people who have trouble digesting it.
- Artificial sweeteners. Sorbitol, erythritol and mannitol — artificial sweeteners are nonabsorbable sugars found in chewing gum and other sugar-free products — can cause diarrhea in some otherwise healthy people.
- Surgery. Partial intestine or gallbladder removal surgeries can sometimes cause diarrhea.
- Other digestive disorders. Chronic diarrhea has a number of other causes, such as IBS, Crohn's disease, ulcerative colitis, celiac disease, microscopic colitis and small intestinal bacterial overgrowth (SIBO).
Complications
Diarrhea can cause dehydration, which can be life-threatening if untreated. Dehydration is particularly dangerous in children, older adults and those with weakened immune systems.
If you have signs of serious dehydration, seek medical help.
Indications of dehydration in adults
These include:
- Excessive thirst.
- Dry mouth or skin.
- Little or no urination.
- Weakness, dizziness or lightheadedness.
- Fatigue.
- Dark-colored urine.
Indications of dehydration in infants and young children
These include:
- Not having a wet diaper in three or more hours.
- Dry mouth and tongue.
- Fever above 102 F (39 C).
- Crying without tears.
- Drowsiness, unresponsiveness or irritability.
- Sunken appearance to the belly, eyes or cheeks.
Prevention
Preventing infectious diarrhea
Wash your hands to prevent the spread of infectious diarrhea. To ensure adequate hand-washing:
- Wash frequently. Wash your hands before and after preparing food. Wash your hands after handling uncooked meat, using the toilet, changing diapers, sneezing, coughing and blowing your nose.
- Lather with soap for at least 20 seconds. After putting soap on your hands, rub your hands together for at least 20 seconds. This is about as long as it takes to sing "Happy Birthday" twice through.
- Use hand sanitizer when washing isn't possible. Use an alcohol-based hand sanitizer when you can't get to a sink. Apply the hand sanitizer as you would hand lotion, making sure to cover the fronts and backs of both hands. Use a product that contains at least 60% alcohol.
Vaccination
You can help protect your infant from rotavirus, the most common cause of viral diarrhea in children, with one of two approved vaccines. Ask your baby's doctor about having your baby vaccinated.
Preventing traveler's diarrhea
Diarrhea commonly affects people who travel to countries where there's inadequate sanitation and contaminated food. To reduce your risk:
- Watch what you eat. Eat hot, well-cooked foods. Don't eat raw fruits and vegetables unless you can peel them yourself. Don't eat raw or undercooked meats and dairy foods.
-
Watch what you drink. Drink bottled water, soda, beer or wine served in its original container. Don't drink tap water or use ice cubes. Use bottled water even for brushing your teeth. Keep your mouth closed while you shower.
Beverages made with boiled water, such as coffee and tea, are probably safe. Remember that alcohol and caffeine can aggravate diarrhea and worsen dehydration.
- Ask your health care team about antibiotics. If you're traveling to a developing country for an extended time, ask a member of your health care team about antibiotics before you go, especially if you have a weakened immune system.
- Check for travel warnings. The Centers for Disease Control and Prevention maintains a travelers' health website where disease warnings are posted for various countries. If you're planning to travel outside of the United States, check there for warnings and tips for reducing your risk.
Diagnosis
Your health care professional will ask about your medical history, review the medications you take, conduct a physical exam and may order tests to determine what's causing your diarrhea. Possible tests include:
- Blood test. A complete blood count test, measurement of electrolytes and kidney function tests can help indicate the severity of your diarrhea.
- Stool test. Your doctor might recommend a stool test to see if a bacterium or parasite is causing your diarrhea.
- Hydrogen breath test. This type of test can help determine if you have a lactose intolerance. After you drink a liquid that contains high levels of lactose, your breath is measured for hydrogen at regular intervals. Breathing out too much hydrogen indicates that you aren't fully digesting and absorbing lactose.
- Flexible sigmoidoscopy or colonoscopy. Using a thin, lighted tube that's inserted in your rectum, your doctor can see inside your colon. The device is also equipped with a tool that allows your doctor to take a small sample of tissue, called a biopsy, from your colon. Flexible sigmoidoscopy provides a view of the lower colon, while colonoscopy allows the doctor to see the entire colon.
- Upper endoscopy. Doctors use a long, thin tube with a camera on the end to examine your stomach and upper small intestine. They may remove a tissue sample for analysis in the laboratory.
Treatment
Most cases of acute diarrhea clear on their own within a couple of days without treatment. If you've tried lifestyle changes and home remedies for diarrhea without success, your doctor might recommend medicines or other treatments.
Antibiotics or anti-parasitics
Antibiotics or anti-parasitic medicines might help treat diarrhea caused by bacteria or parasites. If a virus is causing your diarrhea, antibiotics won't help.
Treatment to replace fluids
Your doctor likely will advise you to replace the fluids and salts. For most adults, that means drinking water with electrolytes, juice or broth. If drinking liquids upsets your stomach or causes vomiting, your doctor might recommend getting IV fluids.
Water is a good way to replace fluids, but it doesn't contain the salts and electrolytes — minerals such as sodium and potassium — that are essential for your body to function. You can help maintain your electrolyte levels by drinking fruit juices for potassium or eating soups for sodium. But certain fruit juices, such as apple juice, might make diarrhea worse.
For children, ask your doctor about using an oral rehydration solution, such as Pedialyte, to prevent dehydration or replace lost fluids.
Adjusting medicines you're taking
If your doctor determines that an antibiotic caused your diarrhea, they might lower your dose or switch to another medicine.
Treating underlying conditions
If your diarrhea is caused by a more serious condition, such as inflammatory bowel disease, your doctor will work to control that condition. You might be referred to a specialist, such as a gastroenterologist, who can help devise a treatment plan for you.
Lifestyle and home remedies
Diarrhea usually clears up quickly without treatment. To help you cope with your symptoms until the diarrhea goes away, try to do the following:
- Drink plenty of liquids, including water, broths and juices. Avoid caffeine and alcohol.
- Add semisolid and low-fiber foods gradually as your bowel movements return to normal. Try soda crackers, toast, eggs, rice or chicken.
- Don't eat certain foods such as dairy products, fatty foods, high-fiber foods or highly seasoned foods for a few days.
-
Ask about anti-diarrheal medicines. Nonprescription anti-diarrheal medicines, such as loperamide and bismuth subsalicylate, might help reduce the number of watery bowel movements and control severe symptoms.
Certain medical conditions and infections — bacterial and parasitic — can be worsened by these medicines because they prevent your body from getting rid of what's causing the diarrhea. Some of these medicines are not recommended for children. Check with your doctor before taking these medicines or giving them to a child.
- Consider taking probiotics. These microorganisms may help restore a healthy balance to the intestinal tract by boosting the level of good bacteria. However, it's not clear if they can help shorten a bout of diarrhea. Probiotics are available in capsule or liquid form and are also added to some foods, such as certain brands of yogurt. Further research is needed to better understand which strains of bacteria are most helpful or what doses are needed.
Preparing for an appointment
You might start by seeing a member of your primary health care team. If you have persistent diarrhea, you may be referred to a doctor who specializes in the digestive system, called a gastroenterologist.
Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fast before certain tests. Make a list of:
- Your symptoms, including when they began and any that may seem unrelated to the reason for which you scheduled the appointment.
- Key personal information, including any major stresses, recent life changes or travel.
- Medications, vitamins or supplements you take, including doses. If you've recently taken an antibiotic, note what kind, for how long and when you stopped.
- Questions to ask your doctor.
For diarrhea, some basic questions to ask include:
- What is likely causing my diarrhea?
- Could my diarrhea be caused by a medicine I'm taking?
- What tests do I need?
- Is my diarrhea likely temporary or chronic?
- What is the best course of action?
- What are the alternatives to the primary approach that you're suggesting?
- I have other health conditions. How can I best manage them with the diarrhea?
- Are there restrictions I should follow?
- May I take medicine such as loperamide to slow the diarrhea down?
- Should I see a specialist?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you questions, including:
- When did your symptoms begin?
- Have your symptoms been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Does your diarrhea awaken you at night?
- Do you see blood, or are your bowel movements black in color?
- Have you recently been around anyone who has diarrhea?
- Have you recently stayed in a hospital or nursing home?
- Have you taken antibiotics recently?
What you can do in the meantime
While you wait for your appointment, you may ease your symptoms if you:
- Drink more fluids. To help avoid dehydration, drink water, juice and broth.
- Don't eat foods that can aggravate diarrhea. Stay away from fatty, high-fiber or highly seasoned foods.
Last Updated Aug 22, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



