Reactive arthritis
Overview
Reactive arthritis is joint pain and swelling triggered by an infection in another part of the body — most often the intestines, genitals or urinary tract.
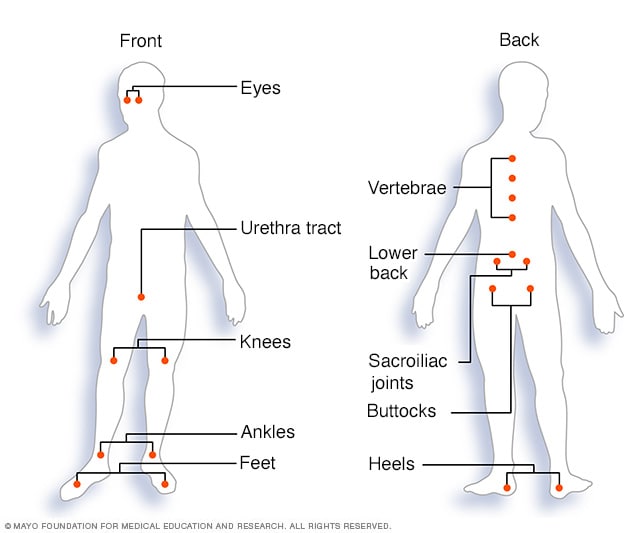
This condition usually targets the knees, ankles and feet. Inflammation also can affect the eyes, skin and the tube that carries urine out of the body (urethra). Previously, reactive arthritis was sometimes called Reiter's syndrome.
Reactive arthritis isn't common. For most people, signs and symptoms come and go, eventually disappearing within 12 months.
Symptoms
The signs and symptoms of reactive arthritis generally start 1 to 4 weeks after exposure to a triggering infection. They might include:
- Pain and stiffness. The joint pain associated with reactive arthritis most commonly occurs in the knees, ankles and feet. Pain may also occur in the heels, low back or buttocks.
- Eye inflammation. Many people who have reactive arthritis also develop eye inflammation (conjunctivitis).
- Urinary problems. Increased frequency and discomfort during urination may occur, as can inflammation of the prostate gland or cervix.
- Inflammation of tendons and ligaments where they attach to bone (enthesitis). This happens most often in the heels and the sole of the feet.
- Swollen toes or fingers. In some cases, toes or fingers might become so swollen that they look like sausages.
- Skin problems. Reactive arthritis can affect skin in a variety of ways, including mouth sores and a rash on the soles of the feet and palms of the hands.
- Low back pain. The pain tends to be worse at night or in the morning.
When to see a doctor
If you develop joint pain within a month of having diarrhea or a genital infection, contact your health care provider.
Causes
Reactive arthritis develops in reaction to an infection in your body, often in your intestines, genitals or urinary tract. You might not be aware of the triggering infection if it causes mild symptoms or none at all.
Numerous bacteria can cause reactive arthritis. Some are transmitted sexually, and others are foodborne. The most common ones include:
- Campylobacter
- Chlamydia
- Clostridioides difficile
- Escherichia coli
- Salmonella
- Shigella
- Yersinia
Reactive arthritis isn't contagious. However, the bacteria that cause it can be transmitted sexually or in contaminated food. Only a few of the people who are exposed to these bacteria develop reactive arthritis.
Risk factors
Certain factors increase your risk of reactive arthritis:
- Age. Reactive arthritis occurs most frequently in adults between the ages of 20 and 40.
- Sex. Women and men are equally likely to develop reactive arthritis in response to foodborne infections. However, men are more likely than are women to develop reactive arthritis in response to sexually transmitted bacteria.
- Hereditary factors. A specific genetic marker has been linked to reactive arthritis. But most people who have this marker never develop the condition.
Prevention
Genetic factors appear to play a role in whether you're likely to develop reactive arthritis. Though you can't change your genetic makeup, you can reduce your exposure to the bacteria that may lead to reactive arthritis.
Store your food at proper temperatures and cook it properly. Doing these things help you avoid the many foodborne bacteria that can cause reactive arthritis, including salmonella, shigella, yersinia and campylobacter. Some sexually transmitted infections can trigger reactive arthritis. Use condoms to help lower your risk.
Diagnosis
During the physical exam, your doctor is likely to check your joints for swelling, warmth and tenderness, and test range of motion in your spine and affected joints. Your doctor might also check your eyes for inflammation and your skin for rashes.
Blood tests
Your doctor might recommend that a sample of your blood be tested for:
- Evidence of past or current infection
- Signs of inflammation
- Antibodies associated with other types of arthritis
- A genetic marker linked to reactive arthritis
Joint fluid tests
Your doctor might use a needle to withdraw a sample of fluid from within an affected joint. This fluid will be tested for:
- White blood cell count. An increased number of white blood cells might indicate inflammation or an infection.
- Infections. Bacteria in your joint fluid might indicate septic arthritis, which can result in severe joint damage.
- Crystals. Uric acid crystals in your joint fluid might indicate gout. This very painful type of arthritis often affects the big toe.
Imaging tests
X-rays of your low back, pelvis and joints can indicate whether you have any of the characteristic signs of reactive arthritis. X-rays can also rule out other types of arthritis.
Treatment
The goal of treatment is to manage your symptoms and treat an infection that could still be present.
Medications
If your reactive arthritis was triggered by a bacterial infection, your doctor might prescribe an antibiotic if there is evidence of persistent infection. Which antibiotic you take depends on the bacteria that are present.
Signs and symptoms of reactive arthritis may be eased with:
- Nonsteroidal anti-inflammatory drugs (NSAIDs). Prescription NSAIDs, such as indomethacin (Indocin), can relieve the inflammation and pain of reactive arthritis.
- Steroids. A steroid injection into affected joints can reduce inflammation and allow you to return to your usual activity level. Steroid eye drops may be used for eye symptoms, and steroid creams might be used for skin rashes.
- Rheumatoid arthritis drugs. Limited evidence suggests that medications such as sulfasalazine (Azulfidine), methotrexate (Trexall) or etanercept (Enbrel) can relieve pain and stiffness for some people with reactive arthritis.
Physical therapy
A physical therapist can provide you with targeted exercises for your joints and muscles. Strengthening exercises increase the joint's support by developing the muscles around the affected joints. Range-of-motion exercises can increase your joints' flexibility and reduce stiffness.
Preparing for your appointment
You'll likely start by seeing your primary care provider, who might refer you to a doctor who specializes in arthritis (rheumatologist) for further evaluation.
What you can do
When you make the appointment, ask if there's anything you need to do in advance, such as fasting before having a specific test. Make a list of:
- Your symptoms, including any that seem unrelated to the reason for your appointment
- Key personal information, including your medical history and your family's medical history
- All medications, vitamins or other supplements you take, including doses
- Questions to ask the doctor
Take a family member or friend along, if possible, to help you remember the information you're given. For reactive arthritis, basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- What are other possible causes?
- What tests do I need?
- What treatment approach do you recommend?
- How soon do you expect my symptoms to improve with treatment?
- Is there anything I can do now to help relieve my joint pain?
- Am I at risk of long-term complications from this condition?
- I have these other health conditions. How can I best manage them together?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- When did your symptoms begin?
- Have they been continuous or occasional?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
- Have you had a recent infection?
Last Updated Jan 25, 2022
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use




