Atrial fibrillation
Overview
Atrial fibrillation (AFib) is an irregular and often very rapid heart rhythm. An irregular heart rhythm is called an arrhythmia. AFib can lead to blood clots in the heart. The condition also increases the risk of stroke, heart failure and other heart-related complications.
During atrial fibrillation, the heart's upper chambers — called the atria — beat chaotically and irregularly. They beat out of sync with the lower heart chambers, called the ventricles. For many people, AFib may have no symptoms. But AFib may cause a fast, pounding heartbeat, shortness of breath or light-headedness.
Episodes of atrial fibrillation may come and go, or they may be persistent. AFib itself usually isn't life-threatening. But it's a serious medical condition that needs proper treatment to prevent stroke.
Treatment for atrial fibrillation may include medicines, therapy to shock the heart back to a regular rhythm and procedures to block faulty heart signals.
A person with atrial fibrillation also may have a related heart rhythm problem called atrial flutter. The treatments for AFib and atrial flutter are similar.
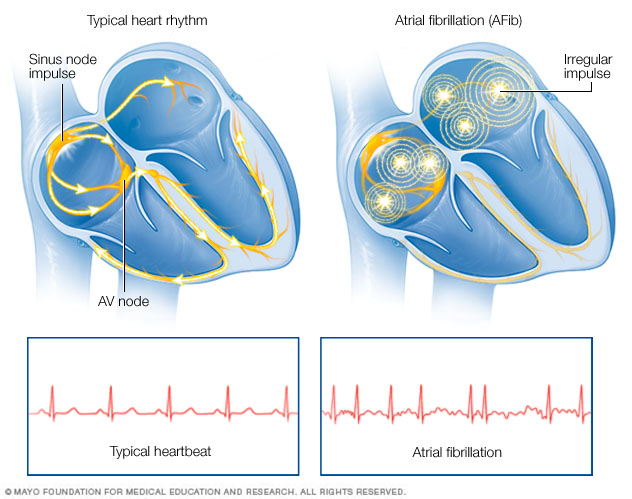
In a typical heart, a tiny group of cells at the sinus node sends out an electrical signal. The signal travels through the heart's upper chambers to the atrioventricular (AV) node. The signal then passes into the lower heart chambers, causing them to squeeze and pump out blood. In atrial fibrillation, electrical signals fire from many locations in the upper chambers, causing them to beat chaotically. Since the AV node doesn't prevent all of these chaotic signals from entering the lower chambers, the heart beats faster and irregularly.
Symptoms
Symptoms of AFib may include:
- Feelings of a fast, fluttering or pounding heartbeat, called palpitations.
- Chest pain.
- Dizziness.
- Fatigue.
- Lightheadedness.
- Reduced ability to exercise.
- Shortness of breath.
- Weakness.
Some people with atrial fibrillation (AFib) don't notice any symptoms.
Atrial fibrillation may be:
- Occasional, also called paroxysmal atrial fibrillation. AFib symptoms come and go. The symptoms usually last for a few minutes to hours. Some people have symptoms for as long as a week. The episodes can happen repeatedly. Symptoms might go away on their own. Some people with occasional AFib need treatment.
- Persistent. The irregular heartbeat is constant. The heart rhythm does not reset on its own. If symptoms occur, medical treatment is needed to correct the heart rhythm.
- Long-standing persistent. This type of AFib is constant and lasts longer than 12 months. Medicines or a procedure are needed to correct the irregular heartbeat.
- Permanent. In this type of atrial fibrillation, the irregular heart rhythm can't be reset. Medicines are needed to control the heart rate and to prevent blood clots.
When to see a doctor
If you have symptoms of atrial fibrillation, make an appointment for a health checkup. You may be referred to a doctor trained in heart diseases, called a cardiologist.
If you have chest pain, seek immediate medical help. Chest pain could mean that you're having a heart attack.
Causes
To understand the causes of atrial fibrillation (AFib), it may be helpful to know how the heart typically beats.
The heart has four chambers:
- The two upper chambers are called the atria.
- The two lower chambers are called the ventricles.
Inside the upper right heart chamber is a group of cells called the sinus node. The sinus node makes the signals that starts each heartbeat.
The signals move across the upper heart chambers. Next, the signals arrive at a group of cells called the AV node, where they usually slow down. The signals then go to the lower heart chambers.
In a healthy heart, this signaling process usually goes smoothly. The resting heart rate is typically 60 to 100 beats a minute.
But in atrial fibrillation, the signals in the upper chambers of the heart are chaotic. As a result, the upper chambers tremble or shake. The AV node is flooded with signals trying to get through to the lower heart chambers. This causes a fast and irregular heart rhythm.
In people with AFib, the heart rate may range from 100 to 175 beats a minute.
Causes of atrial fibrillation
Problems with the heart's structure are the most common cause of atrial fibrillation (AFib).
Heart diseases and health problems that can cause AFib include:
- A heart problem you're born with, called a congenital heart defect.
- A problem with the heart's natural pacemaker, called sick sinus syndrome.
- A sleep disorder called obstructive sleep apnea.
- Heart attack.
- Heart valve disease.
- High blood pressure.
- Lung diseases, including pneumonia.
- Narrowed or blocked arteries, called coronary artery disease.
- Thyroid disease such as an overactive thyroid.
- Infections from viruses.
Heart surgery or stress due to surgery or sickness may also cause AFib. Some people who have atrial fibrillation have no known heart disease or heart damage.
Lifestyle habits that can trigger an AFib episode may include:
- Drinking too much alcohol or caffeine.
- Illegal drug use.
- Smoking or using tobacco.
- Taking medicines that contain stimulants, including cold and allergy medicines bought without a prescription.
Risk factors
Things that can increase the risk of atrial fibrillation (AFib) include:
- Age. The risk of AFib increases as you grow older.
- Caffeine, nicotine or illegal drug use. Caffeine, nicotine and some illegal drugs — such as amphetamines and cocaine — can cause your heart to beat faster. Use of these substances may lead to the development of more-serious arrhythmias.
- Drinking too much alcohol. Drinking too much alcohol can affect the electrical signals in the heart. This can increase the risk of atrial fibrillation.
- Changes in the level of body minerals. Minerals in the blood called electrolytes — such as potassium, sodium, calcium and magnesium — help the heart beat. If these substances are too low or too high, irregular heartbeats may occur.
- Family history. An increased risk of atrial fibrillation occurs in some families.
- Heart problems or heart surgery. Coronary artery disease, heart valve disease and heart problems present at birth increase the risk of AFib. A history of heart attack or heart surgery also makes a person more likely to get the condition.
- High blood pressure. Having high blood pressure increases the risk of getting coronary artery disease. Over time, high blood pressure may cause part of the heart to become stiff and thick. This can change how heartbeat signals travel through the heart.
- Obesity. People who have obesity are at higher risk of developing atrial fibrillation.
- Other long-term health conditions. You may be more likely to get AFib if you have diabetes, chronic kidney disease, lung disease or sleep apnea.
- Some medicines and supplements. Some prescription medicines and certain cough and cold remedies bought without a prescription can cause irregular heartbeats.
- Thyroid disease. Having an overactive thyroid gland can raise the risk of irregular heartbeats.
Complications
Blood clots are a dangerous complication of atrial fibrillation (AFib). Blood clots can lead to stroke.
The risk of stroke from AFib increases as you grow older. Other health conditions also may increase the risk of a stroke due to AFib. These conditions include:
- High blood pressure.
- Diabetes.
- Heart failure.
- Some types of heart valve disease.
Blood thinners are commonly prescribed to prevent blood clots and strokes in people with atrial fibrillation.
Prevention
Healthy lifestyle choices can reduce the risk of heart disease and may prevent atrial fibrillation (AFib). Here are some basic heart-healthy tips:
- Control high blood pressure, high cholesterol and diabetes.
- Don't smoke or use tobacco.
- Eat a diet that's low in salt and saturated fat.
- Exercise at least 30 minutes a day on most days of the week unless your health care team says not to.
- Get good sleep. Adults should aim for 7 to 9 hours daily.
- Maintain a healthy weight.
- Reduce and manage stress.
Diagnosis
You may not know you have atrial fibrillation (AFib). The condition may be found when a health checkup is done for another reason.
To diagnose AFib, the health care provider examines you and asks questions about your medical history and symptoms. Tests may be done to look for conditions that can cause irregular heartbeats, such as heart disease or thyroid disease.
Tests
Tests to diagnose atrial fibrillation (AFib) may include:
- Blood tests. Blood tests are done to look for health conditions or substances that may affect the heart or heartbeat.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. Sticky patches called electrodes are placed on the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which prints or displays the test results. An ECG can show the heart rhythm and how slow or fast the heart is beating. It's the main test for diagnosing atrial fibrillation.
- Holter monitor. This small, portable ECG device records the heart's activity. It's worn for a day or two while you do your regular activities.
- Event recorder. This device is like a Holter monitor, but it records only at certain times for a few minutes at a time. It's typically worn for about 30 days. You usually push a button when you feel symptoms. Some devices automatically record when an irregular heart rhythm is detected.
- Implantable loop recorder. This device records the heartbeat continuously for up to three years. It's also called a cardiac event recorder. The device shows how the heart is beating while you do your daily activities. It may be used to see how often you have an AFib episode. Sometimes it's used to find rare episodes of AFib in those at high risk of the heart problem. For example, you may need one if you've had an unexplained stroke.
- Echocardiogram. Sound waves are used to create images of the beating heart. This test can show how blood flows through the heart and heart valves.
- Exercise stress tests. These tests often involve walking on a treadmill or pedaling a stationary bike while the heart is monitored. The tests show how the heart reacts to exercise. If you can't exercise, you may be given medicine that increases the heart rate like exercise does. Sometimes echocardiogram is done during a stress test.
- Chest X-ray. A chest X-ray shows the condition of the lungs and heart.
Treatment
The goals of atrial fibrillation treatment are to reset and control the heartbeat and prevent blood clots.
Treatment depends on:
- How long you've had AFib.
- Your symptoms.
- The cause of the irregular heartbeat.
Atrial fibrillation treatment may involve:
- Medicine.
- Therapy to reset the heart rhythm, called cardioversion.
- Surgery or catheter procedures.
Together, you and your health care team discuss the best treatment option for you. It's important to follow your atrial fibrillation treatment plan. If AFib isn't well controlled, it may lead to other complications, including stroke and heart failure.
Medications
Treatment for atrial fibrillation may include medicines to do the following:
- Control the speed of the heartbeat.
- Restore the heart rhythm.
- Prevent blood clots, a dangerous complication of AFib.
Medicines that may be used include:
- Beta blockers. These medicines help slow the heart rate.
- Calcium channel blockers. These medicines control the heart rate but may need to be avoided by those who have heart failure or low blood pressure.
- Digoxin. This medicine may control the heart rate at rest, but not as well during activity. Most people need additional or alternative medicines, such as calcium channel blockers or beta blockers.
- Medicines to control the heart rate and rhythm. Also called anti-arrhythmics, this type of medicine is used sparingly. They tend to have more side effects than other medicines to control the heart rate.
- Blood thinners. Also called anticoagulants, these medicines help prevent blood clots and reduce the risk of stroke. Blood thinners include warfarin (Jantoven), apixaban (Eliquis), dabigatran (Pradaxa), edoxaban (Savaysa) and rivaroxaban (Xarelto). If you take warfarin, you'll need to have regular blood tests to monitor the medicine's effects.
Cardioversion therapy
If atrial fibrillation symptoms are bothersome or if this is the first AFib episode, a doctor may try to reset the heart rhythm using a procedure called cardioversion.
Cardioversion can be done in two ways:
- Electrical cardioversion. This method to reset the heart rhythm is done by sending electric shocks to the heart through paddles or patches placed on the chest.
- Drug cardioversion. Medicines given through an IV or by mouth are used to reset the heart rhythm.
Cardioversion is usually done in a hospital as a scheduled procedure. However, it may be done in emergency situations. If it's scheduled, a blood thinner such as warfarin (Jantoven) may need to be taken for a few weeks before the procedure. The medicine reduces the risk of blood clots and strokes.
After electrical cardioversion, medicines to control the heart rhythm may be needed for life to prevent future episodes of atrial fibrillation. Even with medicine, AFib could return.
Surgery or catheter procedures
If AFib doesn't get better with medicine or other treatments, a procedure called cardiac ablation may be necessary. Sometimes ablation is the first treatment.
Cardiac ablation often uses heat or cold energy to create tiny scars in the heart. The scars disrupt irregular heart signals and restore a typical heartbeat. A doctor inserts a flexible tube called a catheter through a blood vessel, usually in your groin, and into your heart. More than one catheter may be used. Sensors on the tip of the catheter apply the cold or heat energy.
Less commonly, ablation is done using a scalpel during open-heart surgery.
There are several types of cardiac ablation. The type used to treat atrial fibrillation depends on your specific symptoms, overall health and whether you're having another heart surgery.
- Atrioventricular (AV) node ablation. Heat energy is usually applied to the heart tissue at the AV node to destroy the electrical signaling connection. After this treatment, a pacemaker is needed for life.
-
Maze procedure. A doctor uses heat or cold energy or a scalpel to create a pattern — or maze – of scar tissue in the upper chambers of the heart. Scar tissue doesn't send electrical signals. So the maze interferes with the stray heart signals that cause atrial fibrillation.
If a scalpel is used to create the maze pattern, open-heart surgery is necessary. This is called the surgical maze procedure. It's the preferred AFib treatment in those who need another heart surgery, such as coronary artery bypass surgery or heart valve repair.
- Hybrid atrial fibrillation ablation. This therapy combines ablation with surgery. It is used to treat long-standing persistent atrial fibrillation.
- Pulsed field ablation. This is a treatment for some types of continued atrial fibrillation. It does not use heat or cold energy. Instead, it uses high energy electric pulses to create areas of scar tissue in the heart. The scar tissue blocks faulty electrical signals that cause AFib.
Atrial fibrillation may return after cardiac ablation. If this happens, another ablation or heart treatment may be recommended. After cardiac ablation, lifelong blood thinners may be needed to prevent strokes.
If you have AFib but can't take blood thinners, you may need a procedure to seal a small sac in the left upper heart chamber. This sac, called an appendage, is where most AFib related clots form. This procedure is called left atrial appendage closure. A closure device is gently guided through a catheter to the sac. Once the device is in place, the catheter is removed. The device stays in permanently. Surgery to close the left atrial appendage also is an option for some people with AFib who are having another heart surgery.
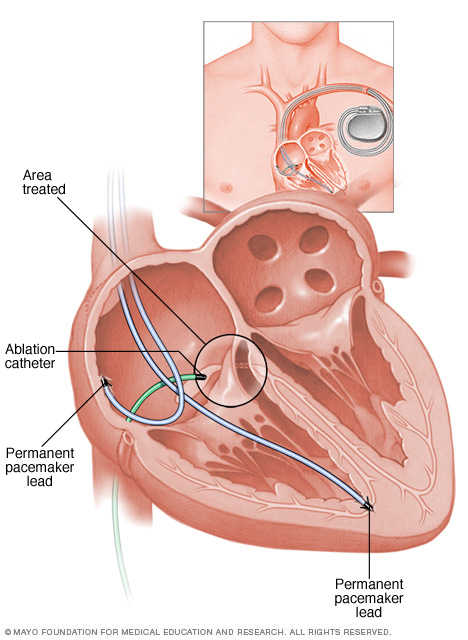
Atrioventricular (AV) node ablation uses heat energy, called radiofrequency energy, to destroy the area between the upper and lower heart chambers. This area is called the AV node. The heart's electrical signals can't pass through the damaged area. So this treatment blocks the faulty heart signals that cause atrial fibrillation (AFib). Once the AV node is destroyed, a pacemaker is needed to control the heart rhythm.
Lifestyle and home remedies
Following a heart-healthy lifestyle can help prevent or treat conditions that can lead to atrial fibrillation (AFib). The following changes are recommended to improve heart health:
- Eat healthy foods. Choose plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats.
- Exercise and stay active. Regular physical activity helps control diabetes, high cholesterol and high blood pressure — all risk factors for heart disease. Try to get 30 to 60 minutes of physical activity most days of the week. Talk to your health care team about the amount and type of exercise that's best for you.
- Don't smoke. Smoking is a major risk factor for heart disease. If you need help quitting, talk to your health care team.
- Maintain a healthy weight. Being overweight increases the risk of heart disease. Talk with your care provider to set realistic goals for weight.
- Control blood pressure. Get your blood pressure checked at least every two years if you're 18 and older. If you have risk factors for heart disease or are over age 40, you may need more-frequent checks. If you have high blood pressure, follow your treatment plan as directed.
- Get your cholesterol checked. Ask your health care team how often you need a cholesterol test. Lifestyle changes and medicines may be recommended to control high cholesterol.
- Limit alcohol. Binge drinking (having five drinks in two hours for men or four drinks for women) can increase the risk of atrial fibrillation. In some people, even lower amounts of alcohol can trigger AFib.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily.
It's also important to have regular health checkups. Tell your health care team if your AFib symptoms get worse.
Preparing for an appointment
If you have an irregular or pounding heartbeat, make an appointment for a health checkup. If AFib is found early, treatment may be easier, and it may work better. You may be referred to a doctor trained in heart diseases. This type of provider is called a cardiologist.
Here's some information to help you prepare for your appointment.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down any symptoms you're having, including any that may seem unrelated to atrial fibrillation. Note when they started, and what you were doing when they started.
- Write down important personal information, including any family history of heart disease, stroke, high blood pressure or diabetes, and any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you're taking — even those bought without a prescription. Include the dosages.
- Take someone along, if possible. Someone who goes with you can help you remember information you're given.
- Write down questions to ask your health care team.
For atrial fibrillation, some basic questions to ask your doctor include:
- What is likely causing my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What kinds of tests will I need?
- What's the most appropriate treatment?
- Is there a generic alternative to the medicine you're prescribing?
- What are other treatment options?
- What foods should I eat or avoid?
- What's an appropriate level of physical activity?
- Are there any other restrictions that I need to follow?
- How often should I be screened for heart disease or complications of AFib?
- I have other health conditions. How can I best manage them together?
- Should I see a specialist?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend visiting?
Don't hesitate to ask any other questions during your appointment.
What to expect from your doctor
During a health checkup, you are usually asked many questions. Being ready to answer them may save time to go over any details you want to spend more time on. You may be asked:
- When did your symptoms start?
- Do you always have symptoms, or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
What you can do in the meantime
It's never too early to make heart-healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. A healthy lifestyle is the main protection against heart problems and heart-related complications.
Last Updated Mar 8, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



