Blocked tear duct
Overview
When you have a blocked tear duct, your tears can't drain normally, leaving you with a watery, irritated eye. The condition is caused by a partial or complete obstruction in the tear drainage system.
A blocked tear duct is common in newborns. The condition usually gets better without any treatment during the first year of life. In adults a blocked tear duct may be due to an injury, an infection or rarely, a tumor.
A blocked tear duct is almost always correctable. Treatment depends on the cause of the blockage and the age of the affected person.
Symptoms
Symptoms of a blocked tear duct include:
- Excessive tearing
- Redness of the white part of the eye
- Recurrent eye infection or inflammation, known as pink eye
- Painful swelling near the inside corner of the eye
- Crusting of the eyelids
- Mucus or pus discharge from the lids and surface of the eye
- Blurred vision
When to see a doctor
See your health care provider if you tear constantly for several days or if your eye is repeatedly or continually infected. A blocked tear duct may be caused by a tumor pressing on the tear drainage system. Early identification of the tumor can give you more treatment options.
Causes
Blocked tear ducts can happen at any age, from birth to adulthood. Causes include:
- Congenital blockage. Many infants are born with a blocked tear duct. The tear drainage system may not be fully developed or there may be a duct abnormality. Often a thin tissue membrane remains over the opening that empties into the nose, called the nasolacrimal duct.
- Age-related changes. As you age, the tiny openings that drain tears, called puncta, may get narrower, causing blockage.
- Infection or inflammation. Long-standing infection or inflammation of your eyes, tear drainage system or nose can cause your tear ducts to become blocked.
- Injury or trauma. An injury to your face can cause bone damage or scarring near the drainage system, affecting the typical flow of tears through the ducts. Even small particles of dirt or loose skin cells lodged in the duct can cause blockage.
- Tumor. A tumor in the nose or anywhere along the tear drainage system can cause blockage.
- Eye drops. Rarely, long-term use of certain medicines, such as eye drops used to treat glaucoma, can cause a blocked tear duct.
- Cancer treatments. A blocked tear duct is a possible side effect of chemotherapy medicine and radiation treatment for cancer.
How the tear drainage system works
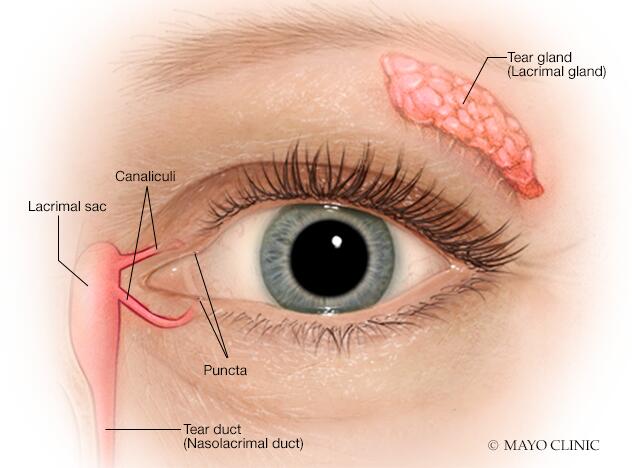
The lacrimal glands produce most of your tears. These glands are located inside the upper lids above each eye. Typically, tears flow from the lacrimal glands over the surface of your eye. Tears drain into openings, called puncta, on the inside corners of your upper and lower eyelids.
The puncta lead to small canals called canaliculi. Canaliculi move tears to a sac to a reservoir on the side of the nose called the lacrimal sac. From there tears travel down the nasolacrimal duct and drain into your nose. Once in the nose, tears are reabsorbed.
A blockage can occur at any point in the tear drainage system, from the puncta to your nose. When that happens, your tears don't drain properly, giving you watery eyes and increasing your risk of eye infections and inflammation.
Risk factors
Certain factors increase your risk of developing a blocked tear duct:
- Age. Older adults are at increased risk of developing blocked tear ducts due to age-related changes.
- Chronic eye inflammation. If your eyes are continually irritated, red and inflamed, you're at higher risk of developing a blocked tear duct.
- Previous surgery. Previous eye, eyelid, nasal or sinus surgery may have caused some scarring of the duct system, possibly resulting in a blocked tear duct later.
- Glaucoma. Anti-glaucoma medicines are often used topically on the eye. If you've used these or other topical eye medicines, you're at higher risk of developing a blocked tear duct.
- Previous cancer treatment. If you've had radiation or chemotherapy to treat cancer, particularly if the radiation was focused on your face or head, you're at higher risk of developing a blocked tear duct.
Complications
Because your tears aren't draining the way they should, the tears that remain in the drainage system become stagnant. This promotes growth of bacteria, viruses and fungi, which can lead to frequent eye infections and inflammation.
Any part of the tear drainage system, including the clear membrane over your eye surface known as the conjunctiva, can become infected or inflamed because of a blocked tear duct.
Prevention
To reduce your risk of developing a blocked tear duct later in life, get prompt treatment of eye inflammation or infections. Follow these tips to avoid eye infections in the first place:
- Wash your hands thoroughly and often.
- Try not to rub your eyes.
- Replace your eyeliner and mascara regularly. Never share these cosmetics with others.
- If you wear contact lenses, keep them clean according to recommendations provided by the manufacturer and your eye care specialist.
Diagnosis
To diagnose your condition, your health care provider talks with you about your symptoms, examines your eyes and does a few tests. Your provider will also examine the inside of your nose to determine if any structural disorders of your nasal passages are causing an obstruction. If your provider suspects a blocked tear duct, you may undergo other tests to find the location of the blockage.
Tests used to diagnose a blocked tear duct include:
- Tear drainage test. This test measures how quickly your tears are draining. One drop of a special dye is placed on the surface of each eye. You may have a blocked tear duct if after five minutes most of the dye is still on the surface of your eye.
- Irrigation and probing. Your provider may flush a saline solution through your tear drainage system to check how well it's draining. Or a slender instrument may be inserted through the tiny drainage holes at the corner of your lid, called puncta, to check for blockages. In some cases this probing may even fix the problem.
- Eye imaging tests. For these procedures, a contrast dye is passed from the puncta in the corner of your lid through your tear drainage system. Then X-ray, computerized tomography (CT) or magnetic resonance imaging (MRI) is used to find the location and cause of the blockage.
Treatment
Your treatment depends on what's causing the blocked tear duct. You may need more than one approach to correct the problem. If a tumor is causing your blocked tear duct, treatment will focus on the cause of the tumor. Surgery may be performed to remove the tumor, or your provider may recommend using other treatments to shrink it.
- Medicines to fight infection. If your provider suspects that an infection is present, antibiotic eye drops or pills may be prescribed.
-
Watch-and-wait or massage. Babies born with a blocked tear duct often get better without any treatment. This can happen as the drainage system matures during the first few months of life. Often a thin tissue membrane remains over the opening that empties into the nose, called the nasolacrimal duct. If your baby's blocked tear duct isn't improving, your baby's health care provider may teach you a special massage technique to help open the membrane.
If you've had a facial injury that caused blocked tear ducts, your provider may suggest waiting a few months to see if the condition improves as your injury heals. As the swelling goes down, your tear ducts may become unblocked on their own.
-
Dilation, probing and flushing. For infants, this technique is done under general anesthesia. The provider enlarges the punctal openings with a special dilation instrument. A thin probe is then inserted through the puncta and into the tear drainage system.
For adults with partially narrowed puncta, your provider may dilate the puncta with a small probe and then flush the tear duct. This is called irrigation. Irrigation is a simple outpatient procedure that often provides at least temporary relief.
- Stenting or intubation. This procedure is usually done using general anesthesia. A thin tube, made of silicone or polyurethane, is threaded through one or both puncta in the corner of your eyelid. These tubes then pass through the tear drainage system into your nose. A small loop of tubing will stay visible in the corner of your eye, and the tubes are generally left in for about three months before they're removed. Possible complications include inflammation from the presence of the tube.
- Balloon catheter dilation. If other treatments haven't worked or the blockage returns, this procedure may be used. It's usually effective for infants and toddlers and also may be used in adults with a partial blockage. First, a general anesthetic is delivered. Then the provider threads a tube, called a catheter, through the tear duct blockage in the nose. The tube holds a deflated balloon on the tip. The balloon is then inflated and deflated a few times to open the blockage.
Surgery
The surgery that's commonly used to treat blocked tear ducts is called dacryocystorhinostomy (DAK-ree-oh-sis-toe-rye-nohs-tuh-me). This procedure opens the passageway for tears to drain out your nose again. You'll be given a general anesthetic, or a local anesthetic if it's performed as an outpatient procedure.
The steps in this procedure vary, depending on the exact location and extent of your blockage, as well as your surgeon's experience and preferences.
- External. With external dacryocystorhinostomy, your surgeon makes an incision on the side of your nose, close to the lacrimal sac. After connecting the lacrimal sac to your nasal cavity and placing a stent in the new passageway, the surgeon closes up the skin incision with a few stitches.
- Endoscopic or endonasal. With this method, your surgeon uses a microscopic camera and other tiny instruments inserted through the nasal opening to your duct system. This method requires no incision so leaves no scar. But the success rates aren't as high as with the external procedure.
Following surgery you'll use a nasal decongestant spray and eye drops to prevent infection and reduce inflammation. After 6 to 12 weeks, you'll return to your provider's office for removal of any stents used to keep the new channel open during the healing process.
Preparing for your appointment
You may start by seeing your primary health care provider. You may then be referred to a doctor who specializes in treating disorders of the eye, called an ophthalmologist. In some instances, your eye doctor may refer you to someone who specializes in ophthalmic plastic surgery for the eye.
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment make a list of:
- Symptoms you've been having, including any that may seem unrelated to the reason for which you scheduled the appointment.
- All medicines, vitamins and supplements you take, including doses.
- Any eye drops that you've been taking.
- Questions to ask your health care provider.
For a blocked tear duct, some basic questions to ask include:
- What's the most likely cause of my symptoms?
- Are there other possible causes?
- Do I need any tests?
- How long will my condition last?
- What treatments are available, and which do you recommend?
- What side effects can I expect from treatment?
- Is this condition related to another medical disorder?
- If I don't have anything done to correct this problem, what are the risks to my vision?
- Do you have any brochures or other printed materials that I can take with me? What websites do you recommend?
What to expect from your doctor
Your provider is likely to ask you a number of questions, such as:
- When did your symptoms begin?
- Do you experience your symptoms all the time, or do they come and go?
- Does anything relieve your symptoms?
- Have you used any eye drops for this problem?
- Have you had any previous surgery to your eyes or eyelid?
- Have you had facial trauma, injuries, radiation treatment or surgery?
- Have you ever had any facial nerve conditions, such as Bell's palsy?
- Do you have any medical problems, such as diabetes or long-standing skin disorders, such as atopic dermatitis?
- Have you ever been diagnosed with a thyroid disorder?
- Do you use contact lenses? Have you used contacts in the past?
Last Updated Mar 8, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



