Sciatica
Overview
Sciatica refers to pain that travels along the path of the sciatic nerve. The sciatic nerve travels from the buttocks and down each leg.
Sciatica most often happens when a herniated disk or an overgrowth of bone puts pressure on the lumbar spine nerve roots. This happens "upstream" from the sciatic nerve. This causes inflammation, pain and often some numbness in the affected leg.
Although the pain associated with sciatica can be serious, those cases that are caused by a herniated disk can clear up with treatment in a few weeks to months. People who have severe sciatica and serious leg weakness or bowel or bladder changes might need surgery.
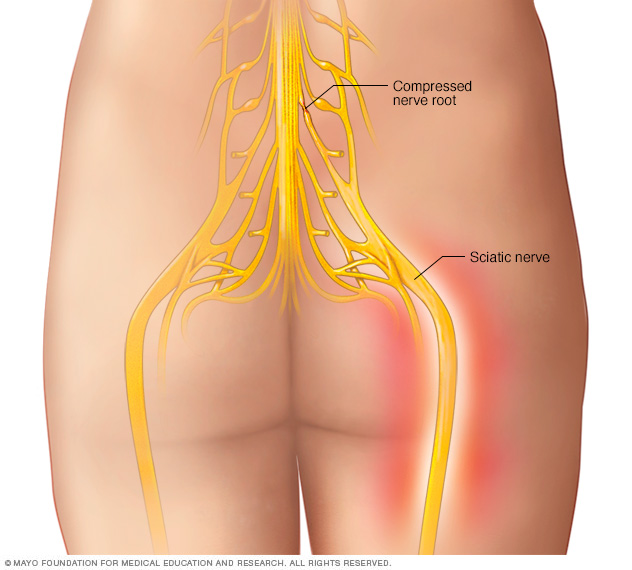
The sciatic nerve is the confluence of nerve roots from the lower back. The sciatic nerve extends from the buttocks down each leg.
Symptoms
Sciatica pain can be almost anywhere along the nerve pathway. It's especially likely to follow a path from the low back to the buttock and the back of a thigh and calf.
The pain can vary from a mild ache to a sharp, burning pain. Sometimes it feels like a jolt or electric shock. It can be worse when coughing or sneezing or sitting a long time. Usually, sciatica affects only one side of the body.
Some people also have numbness, tingling, or muscle weakness in the leg or foot. One part of the leg can be in pain, while another part can feel numb.
When to see a doctor
Mild sciatica usually goes away over time. Call your primary care professional if self-care measures don't ease symptoms. Also call if pain lasts longer than a week, is severe or gets worse. Get immediate medical care for:
- Sudden numbness or muscle weakness in a leg.
- Pain after a violent injury, such as a traffic accident.
- Trouble controlling bowels or bladder.
Causes
Sciatica occurs when the nerve roots to the sciatic nerve become pinched. The cause is usually a herniated disk in the spine or an overgrowth of bone, sometimes called bone spurs, on the spinal bones. More rarely, a tumor can put pressure on the nerve.
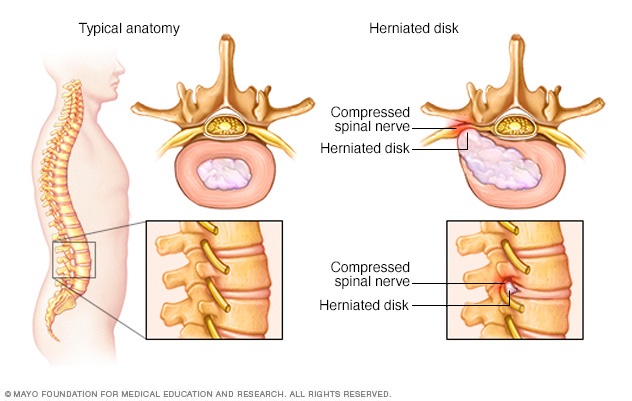
The disks that lie between the vertebrae in the spine consist of a soft center (nucleus) surrounded by a tougher exterior (annulus). A herniated disk occurs when a portion of the nucleus pushes through a crack in the annulus. Symptoms may occur if the herniation compresses a nerve.
Risk factors
Risk factors for sciatica include:
- Age. People ages 20 to 50 are most likely to have herniated disks. Bone spurs develop more commonly as people age.
- Obesity. Being overweight increases stress on the spine.
- Occupation. A job that requires twisting the back, carrying heavy loads or driving a motor vehicle for long periods might play a role in herniated disks.
- Prolonged sitting. People who sit a lot or don't move much are more likely to develop herniated disks than active people are.
- Diabetes. This condition, which affects the way the body uses blood sugar, increases the risk of nerve damage.
Complications
Most people recover fully from sciatica caused by herniated disks, often without treatment. But sciatica can damage nerves. Seek immediate medical attention for:
- Loss of feeling in the affected leg.
- Weakness in the affected leg.
- Loss of bowel or bladder control.
Prevention
It's not always possible to prevent sciatica, and the condition can come back. To protect your back:
- Exercise regularly. To keep the back strong, work the core muscles — the muscles in the abdomen and lower back needed for good posture and alignment. A healthcare professional can recommend activities.
- Keep good posture when sitting. Choose a seat with good lower back support, armrests and a swivel base. For better low back support, place a pillow or rolled towel in the small of the back to keep its normal curve. Keep knees and hips level.
- Use your body correctly. When standing for long periods, rest one foot on a stool or small box from time to time. When lifting something heavy, let your legs do the work. Hold the load close to your body. Don't lift and twist at the same time. Find someone to help lift heavy or awkward things.
Diagnosis
During the physical exam, a healthcare professional might check muscle strength and reflexes. For example, you may be asked to walk on your toes or heels, rise from a squatting position, and lift your legs one at a time while lying on your back.
Tests
People with severe pain or pain that doesn't improve within a few weeks may need:
- X-ray. An X-ray of the spine may reveal various mechanical changes that can affect the size of the holes where the nerve roots exit the spine.
- MRI. This procedure uses a powerful magnet and radio waves to produce cross-sectional images of the back. An MRI produces detailed images of the soft tissues, so herniated disks and pinched nerves show on the scan.
- CT scan. Having a CT scan might involve having a dye injected into the spinal canal before the X-rays are taken (CT myelogram). The dye then moves around the spinal cord and spinal nerves, making them easier to see on the images.
- Electromyography (EMG). This test measures the electrical impulses produced by the nerves and the responses of the muscles. This test can confirm how severe a nerve root injury is.
Treatment
For pain that doesn't improve with self-care measures, some of the following treatments might help.
Medications
The types of medicines that might be used to treat sciatica pain include:
- Anti-inflammatories.
- Corticosteroids.
- Antidepressants.
- Anti-seizure medications.
- Opioids.
Physical therapy
Once the pain improves, a healthcare professional can design a program to help prevent future injuries. This typically includes exercises to correct posture, strengthen the core and improve range of motion.
Steroid injections
In some cases, a shot of a corticosteroid medication into the area around the nerve root that's causing pain can help. Often, one injection helps reduce pain. Up to three can be given in one year.
Surgery
Surgeons can remove the bone spur or the portion of the herniated disk that's pressing on the nerve. But surgery is usually done only when sciatica causes severe weakness, loss of bowel or bladder control, or pain that doesn't improve with other treatments.
Lifestyle and home remedies
For most people, sciatica responds to self-care measures. Although resting for a day or so may provide relief, staying inactive will make symptoms worse.
Other self-care treatments that might help include:
- Cold packs. Place a cold pack on the painful area for up to 20 minutes several times a day. Use an ice pack or a package of frozen peas wrapped in a clean towel.
- Hot packs. After 2 to 3 days, apply heat to the areas that hurt. Use hot packs, a heat lamp or a heating pad on the lowest setting. For continuing pain, try using both warm and cold packs, one at a time.
- Stretching. Stretching exercises for the low back might provide some relief. Try to hold the stretch for at least 30 seconds. Avoid jerking, bouncing or twisting during the stretch.
- Medications. Pain relievers such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) are sometimes helpful for sciatica. Use only as directed.
Alternative medicine
Alternative therapies often used for low back pain include:
- Acupuncture. The acupuncturist inserts hair-thin needles into the skin at certain points on the body. Some studies have suggested that acupuncture can help back pain, while others have found no benefit. If you decide to try acupuncture, choose a licensed professional.
- Chiropractic. Chiropractors can make spinal adjustments or manipulations to restore spinal movement and decrease pain. Spinal manipulation appears to work and to be as safe as standard treatments for low back pain.
- Massage therapy. Massages can help loosen up the larger muscles in the back and hips that may be tight or have spasms.
Preparing for an appointment
Not everyone who has sciatica needs medical care. If your symptoms are serious or last for more than a month, make an appointment with your healthcare professional.
What you can do
- Write down your symptoms and when they began.
- List key medical information, including other conditions you have and the names and doses of medications, vitamins or supplements you take.
- Note recent accidents or injuries that might have damaged your back.
- Take a family member or friend along, if possible. Someone who accompanies you can help you remember the information you get.
- Write down questions to ask your healthcare professional.
For radiating low back pain, some basic questions to ask include:
- What's the most likely cause of my back pain?
- Are there other possible causes?
- What tests do I need?
- What treatment do you recommend?
- Should I have surgery? Why or why not?
- Are there restrictions I need to follow?
- What self-care measures should I take?
- What can I do to keep my symptoms from coming back?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- Do you have numbness or weakness in your legs?
- Do some body positions or activities make your pain better or worse?
- How much does your pain limit your activities?
- Do you do heavy physical work?
- Do you exercise regularly? If yes, with what types of activities?
- What treatments or self-care measures have you tried? Has anything helped?
Last Updated Jan 31, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use



