X-linked agammaglobulinemia
Overview
X-linked agammaglobulinemia (a-gam-uh-glob-u-lih-NEE-me-uh), also called XLA, is an immune system disorder that's passed through families, called inherited. XLA makes it hard to fight infections. People with XLA might get infections of the inner ear, sinuses, respiratory tract, bloodstream and internal organs.
XLA almost always affects males. But females can carry the genes linked to the condition. Most people with XLA are diagnosed in infancy or early childhood, after they've had repeated infections. Some people aren't diagnosed until they're adults.
Symptoms
Most babies with XLA appear healthy for the first few months. They're protected by the proteins called antibodies they got from their mothers before birth.
When these antibodies leave their systems, the babies begin to get repeat bacterial infections. The infections can be life-threatening. Infections might involve the ears, lungs, sinuses and skin.
Male infants born with XLA have:
- Very small tonsils.
- Small or no lymph nodes.
Causes
X-linked agammaglobulinemia is caused by a change in a gene. People with the condition can't produce proteins called antibodies that fight infection. About 40% of people with the condition have a family member who has it.
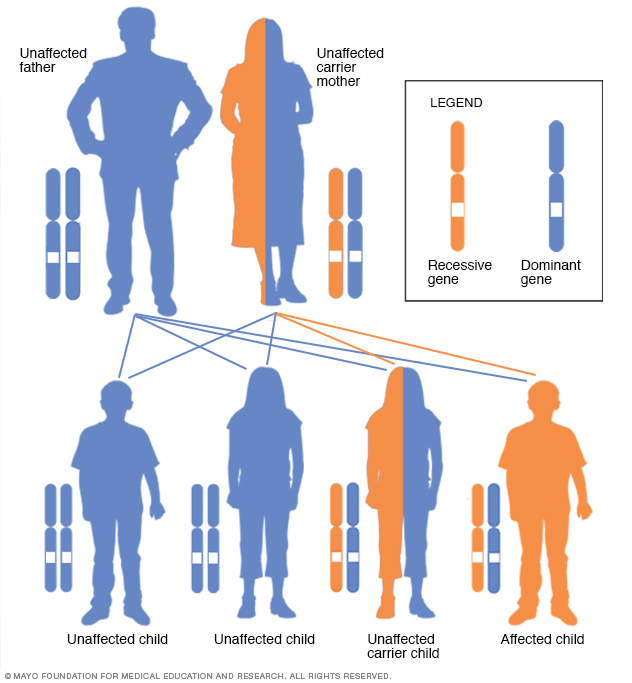
Women can pass down X-linked recessive disorders such as X-linked agammaglobulinemia. Women who are carriers of an X-linked recessive disorder have a 25% chance of having an unaffected son, a 25% chance of having an affected son, a 25% chance of having an unaffected daughter and a 25% chance of having a daughter who also is a carrier.
Complications
People with XLA can live mostly typical lives. They should try to take part in regular activities for their ages. But repeat infections linked to XLA will likely need careful watching and treatment. They can damage organs and be life-threatening.
Possible complications include:
- Long-lasting, called chronic, lung disease.
- Increased risk of certain cancers.
- Infectious arthritis.
- Increased risk of central nervous system infections from live vaccines.
Diagnosis
Diagnosis involves a medical history of repeat infections and a physical exam. Blood tests and maybe genetic testing can confirm the diagnosis.
Treatment
There's no cure for XLA. Treatment aims at boosting the immune system to prevent infections. There also is quick treatment for infections as they happen.
Medications
Medicines to treat XLA include:
-
Gammaglobulin. This is a type of protein found in blood that contains antibodies against infections. It's put into a vein, called infusion, every 2 to 4 weeks or given with weekly shots.
Reactions to gammaglobulin can include headache, chills, backache and nausea. Reactions are more likely to happen during a viral infection, such as a cold.
- Antibiotics. Some people with XLA take antibiotics all the time to prevent infections. Others take antibiotics for bacterial infections longer than do people without XLA.
Your healthcare professional likely will suggest that you have follow-up visits every 6 to 12 months to screen for complications of XLA. You'll also likely be told to not get live vaccines, such as live polio, measles-mumps-rubella or chickenpox vaccines.
Last Updated Jan 10, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use




