Heart valve disease
Overview
In heart valve disease, one or more of the valves in the heart doesn't work properly. There are four heart valves. They keep blood flowing through the heart in the correct direction. Sometimes a valve doesn't open or close all the way. This can change how blood flows through the heart to the rest of the body.
Heart valve disease treatment depends on the heart valve affected and the type and severity of the disease. Sometimes surgery is needed to repair or replace the heart valve.
Symptoms
Some people with heart valve disease might not have symptoms for many years. When symptoms occur, they might include:
- Shortness of breath at rest or when active or lying down.
- Fatigue.
- Chest pain.
- Dizziness.
- Swelling of the ankles and feet.
- Fainting.
- Irregular heartbeat.
When to see a doctor
If you have symptoms of possible heart valve disease, make an appointment for a health checkup. You may be referred to a doctor trained in heart diseases, called a cardiologist.
Causes
To understand the causes of heart valve disease, it may be helpful to know how the heart works.
Four valves in the heart keep blood flowing in the right direction. These valves are:
- Aortic valve.
- Mitral valve.
- Pulmonary valve.
- Tricuspid valve.
Each valve has flaps, called leaflets or cusps. The flaps open and close once during each heartbeat. If a valve flap doesn't open or close properly, less blood moves out of the heart to the rest of the body.
Types of heart valve disease include:
- Stenosis. The valve flaps become thick or stiff and sometimes can join together. The valve opening becomes narrowed. Less blood can flow through the narrowed valve.
- Regurgitation. The valve flaps may not close tightly, causing blood to leak backward.
- Prolapse. The valve flaps become stretched out and floppy. They bulge backward like a parachute. This condition can lead to regurgitation.
- Atresia. The valve isn't formed. A solid sheet of tissue blocks the blood flow between the heart chambers. This type usually affects the pulmonary valve.
Some people are born with heart valve disease. This is called congenital heart valve disease. But adults can get heart valve disease too. Causes of heart valve disease in adults may include infections, age-related changes and other heart conditions.
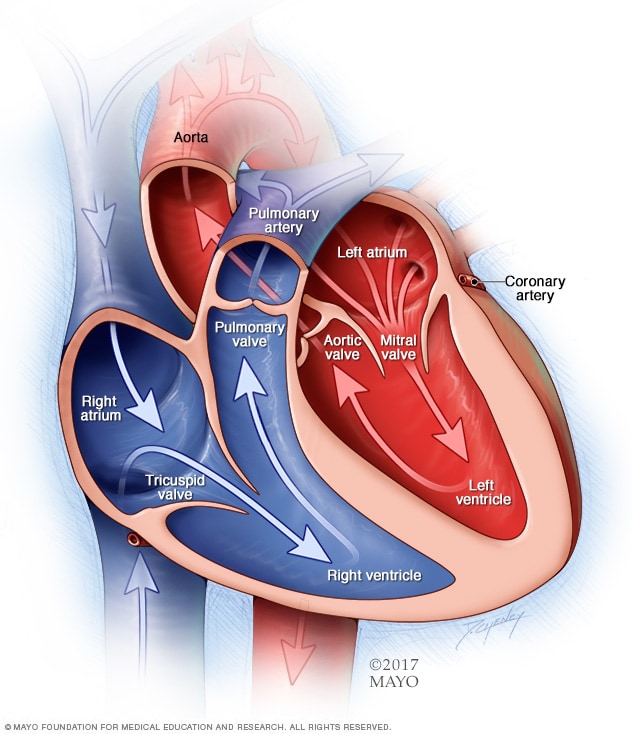
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves are gates at the chamber openings. They keep blood flowing in the right direction.
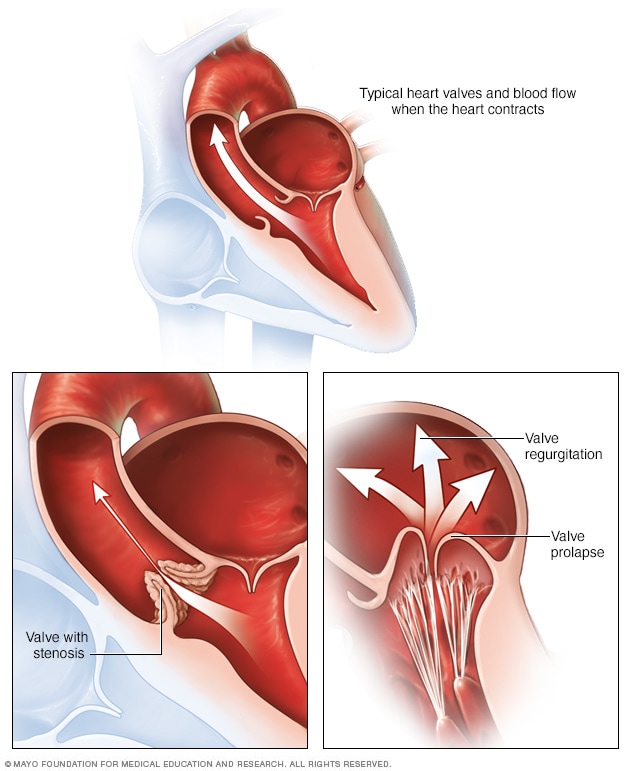
Heart valve disease may include a narrowed valve, called valve stenosis. Sometimes, blood moves backward through a valve. This is called valve regurgitation. If the valve flaps bulge backward, the condition is called valve prolapse.
Risk factors
Several things can increase the risk of heart valve disease, including:
- Older age.
- Some infections, such as rheumatic fever or blood infections.
- A heart attack or some types of heart disease.
- High blood pressure, high cholesterol, diabetes and other heart disease risk factors.
Complications
Heart valve disease can cause many complications, including:
- Heart failure
- Stroke
- Blood clots
- Heart rhythm abnormalities
- Death
Diagnosis
To diagnose heart valve disease, a health care professional examines you and asks questions about your symptoms and health history. A whooshing sound called a heart murmur may be heard when listening to your heart with a device called a stethoscope.
Blood and imaging tests may be done to check your heart health.
Tests
Tests to diagnose heart valve disease may include:
- Echocardiogram. This test uses sound waves to create pictures of the beating heart. It shows how blood flows through the heart and the health of the heart valves. There are different types of echocardiograms. The type you have depends on the reason for the test and your overall health.
- Electrocardiogram (ECG or EKG). This quick test records the electrical signals in the heart. It shows how the heart is beating. Sensors, called electrodes, are attached to the chest and sometimes the legs. Wires connect the sensors to a computer, which displays or prints results.
- Chest X-ray. A chest X-ray shows the heart and lungs. The test can tell if the heart is larger than usual or if there is fluid around the lungs. Fluid could be due to some types of heart valve disease.
- Cardiac MRI. A cardiac MRI uses magnetic fields and radio waves to create detailed images of the heart. It can help determine the severity of heart valve disease.
- Exercise tests or stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is checked. Exercise tests show how the heart responds to physical activity and whether valve disease symptoms occur during exercise. If you can't exercise, you might get medicines that mimic the effect of exercise on the heart.
- Cardiac catheterization. This test isn't often used to diagnose heart valve disease. But it may be done if other tests can't diagnose a heart valve problem. Or it might be used to tell how severe heart valve disease is. A long, thin flexible tube called a catheter is inserted in a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the catheter into the arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video.
Heart valve disease stages
After testing confirms a diagnosis of heart valve disease, your health care team may tell you the stage of disease. Staging helps determine the most appropriate treatment.
The stage of heart valve disease depends on many things, including symptoms, disease severity, the structure of the valve or valves, and blood flow through the heart and lungs.
Heart valve disease is staged into four basic groups:
- Stage A: At risk. Risk factors for heart valve disease are present.
- Stage B: Progressive. Valve disease is mild or moderate. There are no heart valve symptoms.
- Stage C: Asymptomatic severe. There are no heart valve symptoms but the valve disease is severe.
- Stage D: Symptomatic severe. Heart valve disease is severe and is causing symptoms.
Treatment
Heart valve disease treatment depends on:
- The symptoms.
- The severity of the disease.
- If the heart valve problem is getting worse.
Treatment may include:
- Regular health checkups.
- Lifestyle and diet changes.
- Medicines.
- Surgery to repair or replace the valve.
Medications
Some people with heart valve disease need medicines to treat their symptoms. Blood thinners may be given to help prevent blood clots.
Surgery or other procedures
A diseased or damaged heart valve might eventually need to be repaired or replaced, even if you don't have symptoms.
If you need surgery for another heart condition, a surgeon might do valve repair or replacement at the same time.
Methods to repair or replace heart valves include open-heart surgery or minimally invasive heart surgery. Surgeons at some medical centers may do robot-assisted heart valve surgery. The type of heart valve surgery done depends on many things, including age, overall health, and the type and severity of heart valve disease.
Heart valve repair
If you have heart valve disease, your health care team might suggest surgery to repair and save your heart valve. During heart valve repair, the surgeon might:
- Patch holes in a valve.
- Separate valve flaps that have connected.
- Repair the structure of the valve by replacing torn or ruptured cords that support it.
- Remove excess valve tissue so that the valve can close tightly.
- Reduce the outer size of the valve so the flaps can better contact each other.
Heart valve repair procedures include:
- Annuloplasty. A surgeon tightens or reinforces the outer ring around the valve. This surgery may be done with other treatments to repair a heart valve.
- Valvuloplasty. This surgery is used to repair the flaps of the valve. It's often done to repair mitral valve prolapse. The surgeon inserts a flexible tube with a balloon on the tip into an artery in the arm or groin area. The surgeon guides the tube to the affected heart valve. The balloon is inflated. This widens the valve opening. The balloon is deflated, and the tube and balloon are removed. Sometimes clips or plugs are passed through the tube to repair the heart valve.
Heart valve replacement
If a heart valve can't be repaired, surgery may be done to replace it. The most commonly replaced valves are the mitral and aortic valves. A surgeon removes the damaged heart valve and replaces it with one of the following:
- A mechanical valve. This type of artificial heart valve is made of strong material. It also is called a manufactured valve. If you have a mechanical valve, you need blood thinners for life to prevent blood clots.
- A biological valve. This type of artificial heart valve is made from cow, pig or human heart tissue. Biological tissue valves break down over time and eventually need to be replaced.
Sometimes, the aortic valve is replaced with the person's own pulmonary valve. Then the pulmonary valve is replaced with a biological valve. This more complicated surgery is called the Ross procedure.
Valve replacement typically requires open-heart surgery. But less invasive procedures may be available, depending on which heart valve is affected. For example, if the aortic valve is narrowed, surgeons may do transcatheter aortic valve replacement (TAVR). It uses smaller incisions than those used in open-heart surgery.
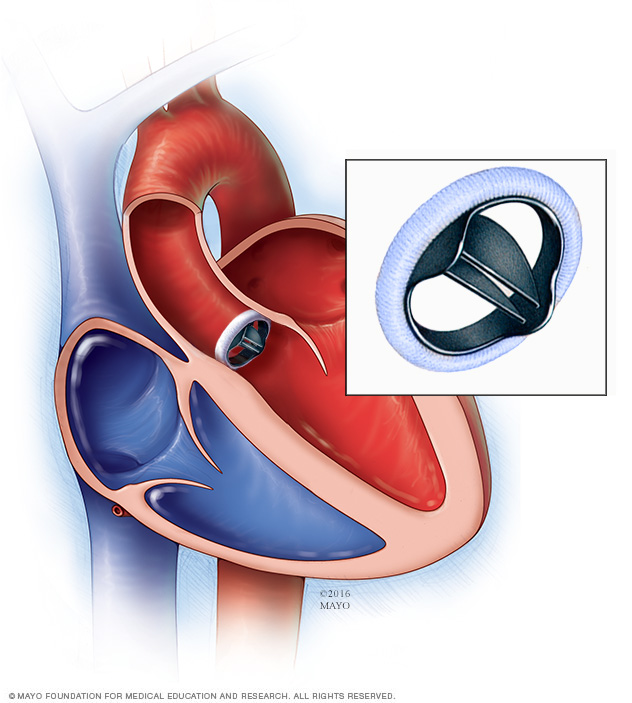
In a mechanical valve replacement, an artificial heart valve made of strong material replaces the damaged valve.
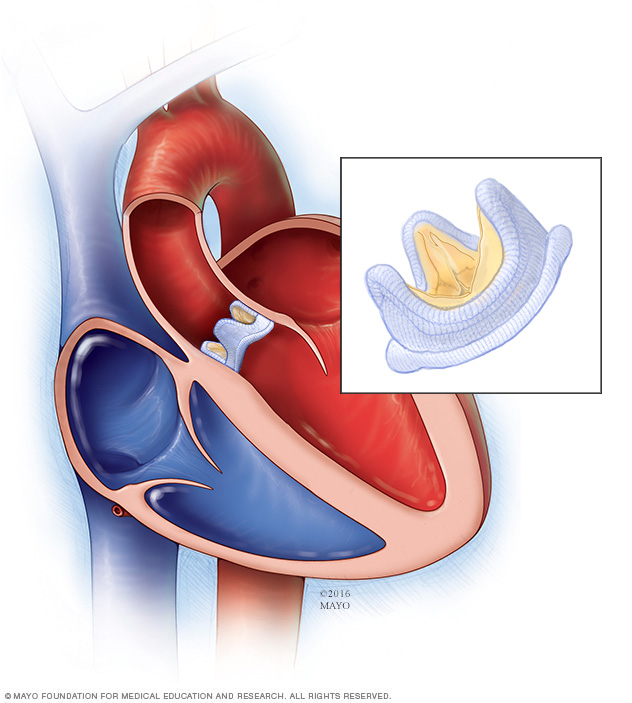
In a biological valve replacement, a valve made from cow, pig or human heart tissue replaces the damaged heart valve.
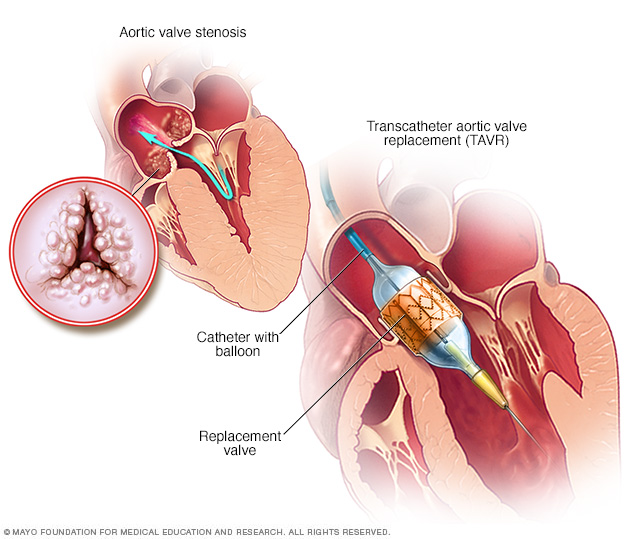
Transcatheter aortic valve replacement (TAVR) is a type of heart valve surgery. It's done to replace a narrowed aortic valve, a condition called aortic valve stenosis. A doctor inserts a flexible tube called a catheter into a blood vessel and guides it into the heart. A replacement valve made of cow or pig tissue goes through the tube to the specific area in the heart. A balloon on the catheter tip inflates to press the new valve into place. Some valves are self-expanding.
Lifestyle and home remedies
If you have heart valve disease, your health care team may suggest making lifestyle changes. Try these steps:
- Eat a heart-healthy diet. Eat a variety of fruits and vegetables, low-fat or fat-free dairy products, poultry, fish, and whole grains. Avoid saturated and trans fats and excess salt and sugar.
- Get regular exercise. As a general goal, aim for at least 30 minutes of moderate physical activity every day. Talk to your health care team before starting a new exercise routine.
- Maintain a healthy weight. Being overweight raises the risk of heart problems. Talk with your care team to set realistic goals for weight.
- Don't use tobacco. If you smoke or chew tobacco, quit. Smoking is a major risk factor for heart disease. Quitting is the best way to reduce the risk. If you need help quitting, talk to a health care professional.
- Practice good sleep habits. Poor sleep may increase the risk of heart disease. Adults should aim to get 7 to 9 hours of sleep daily. Go to bed and wake at the same time every day, including on weekends. If you have trouble sleeping, talk to your health care team about strategies that might help.
- Control blood pressure. Uncontrolled high blood pressure increases the risk of serious health problems. Get your blood pressure checked at least every two years if you're 18 and older. If you have risk factors for heart disease or are over age 40, you may need more-frequent checks.
- Get a cholesterol test. Get a baseline cholesterol test when you're in your 20s and then at least every 4 to 6 years. Some people may need to start testing earlier or have more-frequent checks.
- Manage diabetes. If you have diabetes, tight blood sugar control can help keep your heart healthy.
Pregnancy
Careful and regular checkups are needed for those who have heart valve disease during pregnancy. If you have a severe heart valve condition, you might be told not to get pregnant to reduce the risk of complications.
Coping and support
If you have heart valve disease, here are some ways to help you manage your condition and thrive:
- Get support. Connecting with friends and family or a support group is a good way to reduce stress. You may find that talking about your concerns with others in similar situations can help.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness, and connecting with others in support groups are some ways to reduce and manage stress. If you have anxiety or depression, talk to your health care team about strategies to help.
Preparing for an appointment
If you think you might have symptoms of heart valve disease, make an appointment for a health checkup. Here's some information to help you prepare for your appointment.
What you can do
- Be aware of pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance. For example, you may be told not to eat or drink for a short period before a cholesterol test.
- Write down your symptoms, including any that seem unrelated to heart valve disease.
- Write down important personal information, including a family history of heart valve disease, and any major stresses or recent life changes.
- Make a list of all medicines, vitamins and supplements you take. Include dosages.
- Take someone along, if possible. Someone who goes with you can help you remember information you're given.
- Write down questions to ask your health care team.
For heart valve disease, some basic questions to ask your care team include:
- What is the likely cause of my symptoms or condition?
- What are other possible causes for my symptoms or condition?
- What tests do I need?
- What's the best treatment?
- What are the options to the main treatment that you're suggesting?
- I have other health conditions. How can I best manage them together?
- Are there any activity, sports or diet restrictions I need to follow?
- Should I see a specialist?
- If I need heart valve surgery, which surgeon do you recommend?
- Are there brochures or other printed material I can take with me? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your health care team is likely to ask you many questions, including:
- When did your symptoms begin?
- Do you always have symptoms or do they come and go?
- How severe are your symptoms?
- What, if anything, makes your symptoms better?
- What, if anything, makes your symptoms worse?
Last Updated Nov 22, 2023
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use





